What is a Condylar Fracture?
A condylar fracture refers to a break in the rounded protrusions at the end of a bone, known as condyles, that form part of a joint. These structures are vital for smooth movement and articulation of joints. These are most commonly seen in two major areas: the mandibular condyle in the jaw and the femoral condyle in the knee. Both types are serious because they directly impact a person’s mobility or jaw function.
When a fracture occurs, it usually disrupts the joint surface and can severely impair function. For instance, a mandibular condylar fracture could lead to difficulty speaking, chewing, or even opening the mouth. Meanwhile, a femoral condylar fracture might cause a person to lose mobility in the leg or struggle with walking. These aren’t just simple cracks in the bone; they’re often complicated due to their proximity to vital joint structures.
Furthermore, condylar fractures can be difficult to treat because joints are complex structures with cartilage, ligaments, and blood vessels all tightly packed into one area. If not treated properly, these fractures can lead to chronic pain, deformity, or even permanent loss of function. Early recognition and appropriate treatment are crucial to preventing long-term consequences.
Why Are Condylar Fractures Significant in Orthopedics?
They hold a unique place in orthopedic and maxillofacial medicine because they directly involve the joints, which are essential for movement and function. In orthopedics, preserving joint integrity is a top priority. When the condyle is fractured, the entire biomechanics of the joint can be disrupted. This can result in misalignment, joint instability, and even long-term complications like arthritis or ankylosis (joint stiffness).
One of the most concerning aspects is how easily they can be overlooked. For example, a mandibular condylar fracture may not be immediately visible on standard X-rays. Patients might initially present with symptoms like minor jaw pain or a popping sound, which can easily be mistaken for something less severe, like TMJ disorders. By the time a definitive diagnosis is made, the damage may already be extensive.
These fractures are also significant due to their psychological and social impact. Imagine not being able to eat properly, speak clearly, or walk without pain. These limitations can affect a person’s career, social life, and mental health. That’s why orthopedic and dental professionals take them very seriously and usually work as part of a multidisciplinary team to manage them effectively.
Anatomy of the Condyle
Understanding the Mandibular and Femoral Condyles
The condyle is essentially the rounded end of a bone, and it plays a pivotal role in joint articulation. In humans, the two most commonly discussed condylar areas are the mandibular condyles (located at the ends of the lower jaw) and the femoral condyles (situated at the end of the thigh bone, forming part of the knee joint).
Mandibular condyles connect the jawbone to the skull and are crucial for movements like chewing, speaking, and yawning. They form part of the temporomandibular joint (TMJ)—a complex and delicate structure that allows for multidirectional jaw movement.
On the other hand, femoral condyles are essential components of the knee joint. These rounded projections help in distributing body weight and enabling smooth knee flexion and extension. They’re covered in cartilage to reduce friction and absorb shock during walking or running.
The complexity of the condylar region is what makes fractures in these areas so problematic. Surrounding structures like ligaments, cartilage, nerves, and blood vessels make any surgical or medical intervention a delicate task. A fracture here isn’t just a broken bone—it’s a disruption to an intricate and essential system.
Functions of the Condylar Region
The condylar region doesn’t just support the bone structurally; it plays an active role in every joint movement. In the jaw, this area enables vertical, horizontal, and rotational movements, allowing us to:
- Chew food efficiently
- Talk clearly, and
- Express emotions through facial gestures.
The TMJ is one of the most used joints in the body, making the mandibular condyle especially critical.
In the knee, the femoral condyles bear a huge load every day. They allow the leg to move smoothly during walking, running, squatting, and even standing. Their rounded shape and cartilage covering help in evenly distributing stress across the knee joint. This makes the femoral condyles vital for mobility and stability.
Any injury to this region can cause a cascade of problems. For instance, damage to the cartilage can result in osteoarthritis, while a displaced fracture may change the way the joint fits together, causing chronic pain or reduced range of motion.
Types of Condylar Fractures
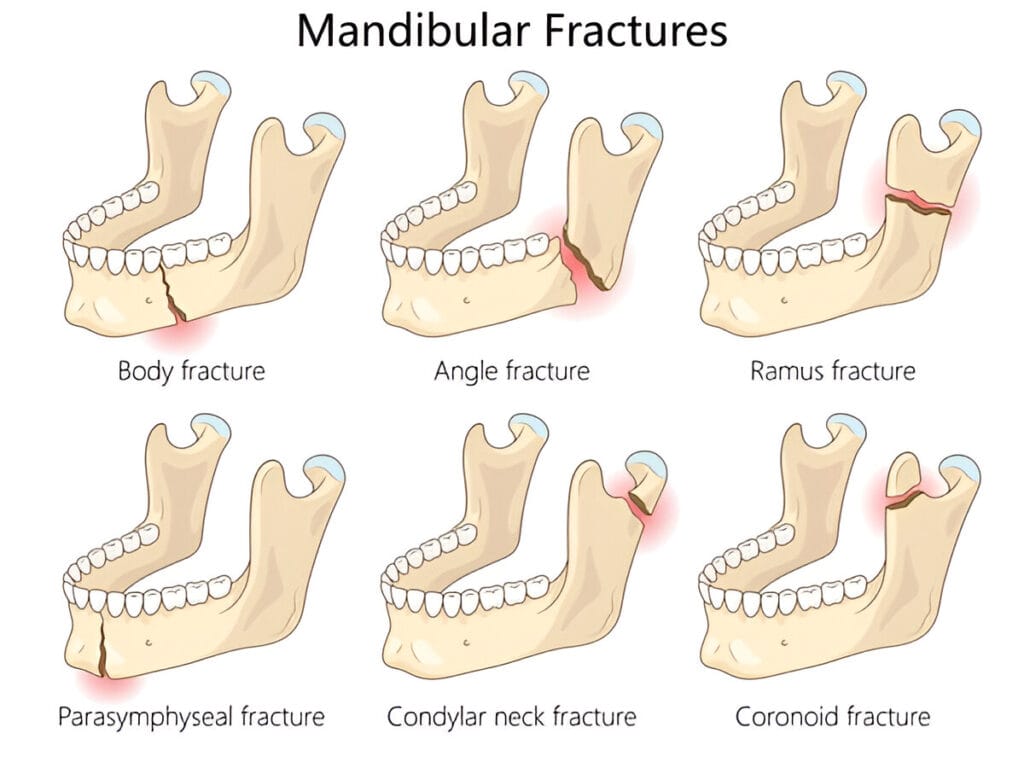
These fractures are classified by location (intracapsular vs. extracapsular), side (unilateral vs. bilateral), and displacement. This classification is essential for guiding treatment and predicting outcomes.
- Intracapsular fractures involve the joint itself and are more prone to complications like stiffness, arthritis, or ankylosis. They often require surgery and extensive rehabilitation.
- Extracapsular fractures, which occur outside the joint capsule, generally have a better prognosis and may be treated conservatively with splints or therapy.
- Unilateral fractures result from trauma to one side of the jaw, causing pain, limited movement, or asymmetry, though the opposite condyle may still function.
- Bilateral fractures, often due to high-impact injuries, are more severe, causing jaw misalignment, restricted opening, and facial deformities, and frequently need surgical correction, especially in children.
- Displaced fractures require surgical realignment to prevent joint dysfunction, bite issues, or chronic disorders.
- Non-displaced fractures may be managed conservatively but still need careful monitoring with imaging to rule out subtle misalignments. Early diagnosis and classification are key to effective treatment and recovery.
Common Causes
Trauma and Accidents
Trauma remains the number one cause, particularly in the context of road traffic accidents, falls, and physical assaults.
- In the case of mandibular condylar fractures, a punch to the side of the face or a car accident where the chin hits the dashboard can transmit enough force to cause the condyle to break.
- For femoral condyles, a high-impact trauma such as a motorcycle accident or a fall from a significant height often leads to complex and sometimes comminuted (shattered) fractures.
These injuries are not just about broken bones; they often come with associated soft tissue damage, including torn ligaments, cartilage injuries, or even nerve damage. This makes diagnosis and treatment more complicated and time-sensitive. Emergency care is often required, and any delay can significantly affect the outcome.
Sports Injuries
Athletes—especially those in contact sports like boxing, football, rugby, and martial arts—are at a significantly higher risk. A misjudged tackle, an elbow to the jaw, or a bad fall can cause direct trauma to the condylar region, leading to a fracture.
Protective gear such as helmets, mouthguards, and knee braces can significantly reduce the risk, but they aren’t foolproof. Prevention also includes proper training, strength conditioning, and using correct techniques during physical activities.
Pathological Weakening of Bones
Not all condylar fractures are caused by trauma. Sometimes, the bones themselves are weakened due to underlying medical conditions, making them more susceptible to fractures even from minor impacts. This is referred to as pathological fractures.
Conditions like osteoporosis, bone tumors, cysts, osteogenesis imperfecta, and even prolonged use of corticosteroids can weaken the bone structure.
Unlike trauma-induced fractures, these often occur without any obvious injury and may go unnoticed for days or even weeks. Diagnosis usually involves not just imaging but also blood tests, bone density scans, and biopsies if tumors or infections are suspected.
Signs and Symptoms to Look Out For
Pain and Swelling
Pain and swelling are often the first and most obvious signs of a condylar fracture. The intensity of pain can vary depending on the severity and location of the fracture.
- With a mandibular condylar fracture, patients typically report a deep, aching pain in the side of the jaw, especially when attempting to chew, speak, or open their mouth. Swelling may be visible along the jawline, and bruising is common.
- In the case of femoral condylar fracture, pain is often sharp and localized to the knee joint. It becomes worse with any attempt to move or bear weight. Swelling is usually rapid and may include joint effusion—where fluid builds up inside the joint capsule, causing a tight, ballooned appearance of the knee.
Importantly, swelling isn’t just a cosmetic concern—it can compress blood vessels and nerves, increasing the risk of complications like compartment syndrome. That’s why any swelling following trauma should be evaluated urgently.
Pain management often includes NSAIDs, cold compresses, and in severe cases, nerve blocks or prescription painkillers. But these are just temporary measures. The underlying fracture must be addressed to provide lasting relief.
Restricted Jaw or Limb Movement
One of the hallmark symptoms of a condylar fracture is restricted movement. This limitation can arise from multiple factors, including pain, mechanical blockage, swelling, or muscle spasms surrounding the injury site.
- In fractures of mandibular condyles, patients often report an inability to open their mouths fully, a condition known as trismus. The lower jaw may also deviate to one side upon opening, depending on which condyle is affected.
- In the case of femoral condylar fractures, restricted movement usually manifests as difficulty in bending or straightening the knee.
Treating this symptom often requires more than just fixing the fracture. After initial stabilization, patients must undergo physical therapy to regain full range of motion. Exercises focus on stretching, strengthening, and gradually increasing movement within safe limits. In some severe or delayed cases, surgical release of adhesions or joint manipulation under anesthesia might be necessary to restore function.
Misalignment and Functional Deficits
One of the most serious complications arising from a condylar fracture is misalignment of the affected joint, which leads to profound functional deficits over time.
- In mandibular fractures, this misalignment often presents as malocclusion, where the teeth no longer fit together correctly. This not only affects chewing efficiency but can also lead to temporomandibular joint dysfunction, chronic pain, and headaches. Over time, if not corrected, it can cause significant cosmetic issues and even speech problems. In severe cases, it may require orthodontic treatment or corrective jaw surgery.
- In fractures of the femoral condyle , misalignment can result in valgus or varus deformities, where the knee tilts inward or outward. This abnormal angulation places uneven stress on the joint, accelerating cartilage wear and increasing the risk of osteoarthritis. Patients may limp, feel unstable while walking, or find it impossible to engage in physical activities without pain.
Correction of misalignment usually requires surgical intervention, particularly if the fracture is displaced. Surgeons may use plates, screws, or even joint replacement components to restore anatomical alignment. Post-operative rehabilitation is critical to ensure that the joint heals in the proper position and regains full functionality.
Functional deficits caused by misalignment are not always reversible, which is why early and accurate management is vital. The longer the joint remains out of alignment, the higher the chances of permanent disability.
Diagnosis of Fractures of Condyles
Clinical Examination
Diagnosis of a condylar fracture begins with a thorough clinical examination. The doctor will assess the patient’s symptoms, inspect the affected area for swelling or bruising, and check for signs like asymmetry, restricted motion, or tenderness.
- In the jaw, the clinician may palpate the condylar region externally and intraorally, asking the patient to open and close their mouth to observe any deviation or clicking sounds. Facial asymmetry, malocclusion, and limited range of motion are red flags that point toward a mandibular condylar fracture.
- In the knee, the examiner will test for joint stability, range of motion, and the presence of joint effusion. Specific stress tests (like the valgus/varus test) may be done to identify associated ligament injuries. A positive patellar tap or balloon sign could indicate fluid accumulation inside the joint capsule—suggestive of an intra-articular injury.
Imaging and Diagnostic Tools
Radiographic imaging plays a crucial role in confirming a condylar fracture and planning treatment. The most commonly used tools include:
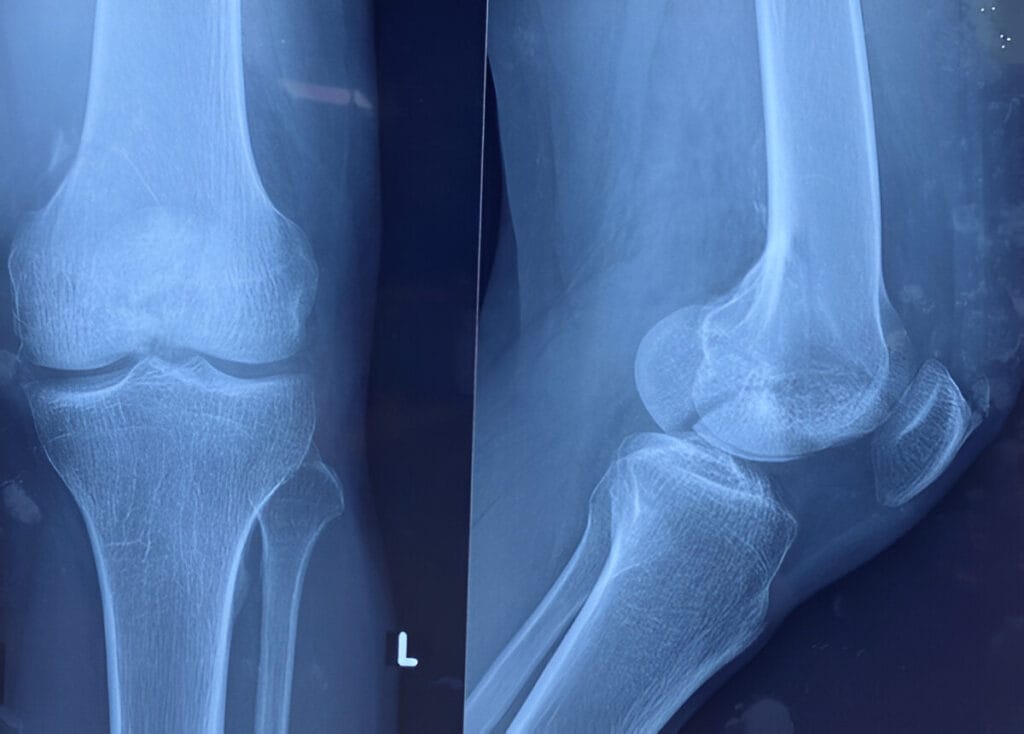
- X-rays: Often the first imaging modality used, especially for assessing bone alignment, a dead piece of bone, and displacement. However, X-rays can sometimes miss hairline or non-displaced fractures, especially in the mandibular condyle, due to overlapping structures.
- CT Scans (Computed Tomography): These provide a more detailed and three-dimensional view of the fracture, helping to assess its extent, displacement, and involvement of the joint surface. CT scans are particularly useful in surgical planning.
- MRI (Magnetic Resonance Imaging): While not typically the first choice, MRIs are excellent for evaluating soft tissue injuries, including ligament tears, cartilage damage, and muscle trauma. In cases where nerve involvement or vascular compromise is suspected, MRI becomes essential.
- Ultrasound: Sometimes used in pediatric cases or when radiation exposure is a concern. It’s non-invasive and useful for identifying effusions and guiding injections.
Combining these tools with clinical examination ensures an accurate diagnosis and effective treatment plan. Imaging not only confirms the presence of a fracture but also helps determine the type, location, and complexity, all of which guide the next steps in care.
Treatment
Treatment depends on the severity, displacement, and the patient’s age or overall health. While minor, non-displaced fractures may heal well with conservative approaches like rest, immobilization, and physical therapy, more complex or displaced fractures often require surgical intervention to restore proper jaw alignment and function. Prompt evaluation by a maxillofacial specialist is essential to determine the best course of action.
Conclusion
Condylar fractures can significantly impact jaw movement, facial symmetry, and knee joint disability if not properly managed. Early diagnosis, appropriate treatment, and rehabilitation play a crucial role in achieving full recovery and minimizing complications. Understanding the signs and seeking timely care can make a lasting difference in outcomes.