A sequestrum is a piece of dead bone that has become separated from the healthy, living bone during the process of necrosis. This condition typically arises as a complication of osteomyelitis, a severe bone infection. When an infection penetrates the bone, the blood supply to part of the bone may be interrupted, leading to tissue death. The necrotic bone, now devoid of circulation, detaches from viable tissue and becomes a sequestrum.
A sequestrum is both a diagnostic clue and a therapeutic challenge. Its presence often signifies a chronic infection that has not responded to antibiotics alone. This makes it an essential focus in the management of chronic osteomyelitis. If left untreated, the sequestrum acts like a foreign object, guarding the infection and potentially causing systemic issues such as sepsis.
Dead bone cannot be resorbed or remodeled like healthy bone tissue. Consequently, surgical removal—termed sequestrectomy—is frequently required. Once removed, the surrounding infected area is typically treated with long-term antibiotics to eradicate the infection.
In summary, understanding what a sequestrum is, and more importantly, what it implies, is critical for timely diagnosis and treatment. It is more than just a complication; it’s a red flag that the underlying infection has progressed and requires aggressive management.
Etymology and Historical Context
The term sequestrum comes from the Latin word sequestrare, meaning “to separate” or “to set aside.” Historically, the term has been used since the early days of surgical medicine when physicians first noticed detached pieces of dead bone in patients suffering from lingering infections. These fragments often protruded through skin ulcers or open wounds, clearly distinct from the surrounding healthy bone.
In the 18th and 19th centuries, sequestrum was a common term in battlefield medicine, where gunshot wounds and poor sanitation led to chronic infections. Surgeons of the time frequently encountered cases where fragments of necrotic bone had to be manually extracted—often without anesthesia.
Today, with advanced imaging and surgical tools, identifying and removing a sequestrum is far more precise. But the ancient medical understanding remains largely the same: a sequestrum signals dead bone and persistent infection.
Causes of Sequestrum Formation
Infection-Related Origins
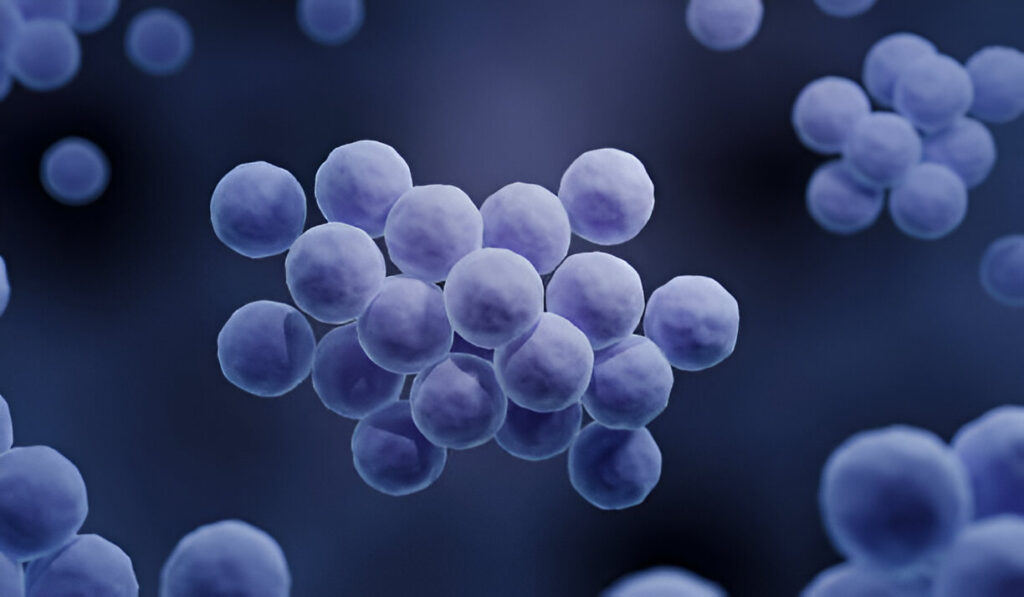
The most common cause of sequestrum formation is infection—specifically, osteomyelitis, which is an inflammation of bone due to a microbial invasion. Bacterial infections, especially those caused by Staphylococcus aureus, can infiltrate the bone via the bloodstream, direct trauma, or adjacent soft tissue infection.
Once inside the bone, the bacteria trigger an immune response. Pus accumulates, pressure builds, and the blood supply to the inner portion of the bone is compromised. This leads to ischemia and bone necrosis. The body’s natural healing processes attempt to wall off the infection by creating a sheath of new bone, called the involucrum, but the dead bone (the sequestrum) remains isolated within.
This infection-driven pathogenesis is why sequestrum is most often seen in cases of chronic osteomyelitis. Acute osteomyelitis, if not treated promptly, can progress into a chronic state where sequestrum formation is inevitable.
Infections following open fractures, post-surgical complications, or contaminated prosthetics are prime culprits. Individuals with compromised immune systems—such as diabetics, cancer patients, and those on immunosuppressive drugs—are particularly at risk.
Trauma-Induced Bone Necrosis
Trauma is another significant factor. When a bone is fractured, particularly in high-impact injuries like car accidents or falls from a height, the vascular supply can be severely disrupted. Without an adequate blood supply, bone cells begin to die, and if infection sets in, a sequestrum may form.
Gunshot wounds and compound fractures are especially high-risk scenarios. Even if infection does not immediately set in, dead bone may remain inside the body, undetected, until secondary infection or chronic inflammation triggers noticeable symptoms. In some cases, the presence of the sequestrum is discovered months or even years later through imaging done for unrelated reasons.
Other Medical Conditions That Lead to Sequestrum
Apart from infections and trauma, other diseases can cause bone tissue to die and form a sequestrum. These include:
- Sickle Cell Anemia: Bone infarctions are common in sickle cell disease, and the resultant necrosis can lead to sequestrum.
- Cancer: Bone tumors, especially osteosarcoma, may disrupt blood supply and cause necrosis.
- Radiation Therapy: Patients receiving radiation near bones (especially in the head and neck) may suffer from radiation osteonecrosis, which can produce sequestra.
- Peripheral Artery Disease (PAD): Reduced blood flow to extremities, especially in diabetic patients, increases the risk of necrotic bone segments.
Understanding the root causes is key to prevention. By managing infections promptly and ensuring proper post-traumatic care, the chances of developing a sequestrum can be significantly reduced.
How Sequestrum Develops in the Body
Pathophysiology and Mechanism
The development of a sequestrum begins when an infection or trauma compromises the bone’s blood supply. Without oxygen and nutrients, the osteocytes (bone cells) die. Unlike soft tissues, bone has a limited capacity for self-repair once its cellular components are necrotic.
The dead bone becomes a foreign body, triggering a cascade of immune responses. White blood cells flood the area, attempting to combat the infection. However, due to the avascular nature of the necrotic segment, antibiotics and immune cells can’t reach it effectively. This isolation allows bacteria to thrive within the dead bone, turning it into a long-term reservoir of infection.
Over time, the body attempts to contain this threat. It begins forming new bone (involucrum) around the dead tissue, essentially walling it off. This process may take weeks to months and is typically seen in chronic osteomyelitis cases.
What results is a pocket of dead bone (the sequestrum) encased in new bone (the involucrum), often with sinus tracts that allow pus to drain externally. This structure can persist indefinitely if not surgically treated.
Differences Between Involucrum and Sequestrum
Though they sound similar, involucrum and sequestrum are opposites in purpose and physiology. The sequestrum is the problem—the dead, infected bone that needs to be removed. The involucrum is the body’s attempt at a solution—a sheath of new bone that tries to isolate the infection and protect the surrounding tissue.
In some cases, the involucrum may become thick enough to trap the sequestrum completely, making surgical removal more complex. On imaging studies, the sequestrum often appears as a dense, irregular bone fragment within a cavity, while the involucrum shows as a smoother outline of new bone.
Understanding these differences is essential for diagnosis, treatment planning, and surgical strategy.
Recognizing the Symptoms of Sequestrum
Common Signs and Patient Complaints
The symptoms of sequestrum can range from mild to severe, depending on the infection’s chronicity and the location of the dead bone. Most commonly, patients report:
- Persistent, deep-seated bone pain
- Swelling and tenderness over the affected area
- Redness and warmth indicating inflammation
- Fever, chills, or malaise in systemic infections
- Non-healing wounds or open draining sinuses
- Foul-smelling discharge from infected sites
In post-surgical or post-traumatic patients, these symptoms may be confused with regular healing pain or inflammation. But if they persist or worsen over time, it’s a strong indicator that a deeper issue, like sequestrum, might be present.
Chronic vs Acute Presentations
Acute presentations are typically seen in newly acquired infections, especially in children, where symptoms like fever and localized swelling appear rapidly. In contrast, chronic sequestrum often presents subtly. Patients may feel fatigue, low-grade fever, or intermittent drainage from a wound months after surgery or injury.
This chronicity makes it easy to overlook or misdiagnose. Only when a persistent infection fails to respond to antibiotics does the investigation for sequestrum typically begin.
Diagnostic Techniques for Identifying Sequestrum
Role of X-rays and MRI
Diagnosing a sequestrum requires a combination of clinical evaluation and imaging studies. Among the imaging modalities, X-rays and Magnetic Resonance Imaging (MRI) are pivotal in identifying and assessing the extent of bone necrosis. PMC
X-rays are often the first imaging technique employed due to their accessibility and cost-effectiveness. In cases of chronic osteomyelitis, X-rays may reveal a sequestrum as a dense, sclerotic area within the bone, often surrounded by a radiolucent zone indicating the presence of granulation tissue or pus. However, early in the disease process, X-rays might not detect subtle changes, as radiographic signs can lag behind clinical symptoms by up to two weeks. NCBI
MRI offers superior sensitivity in detecting early bone marrow changes associated with infection. A sequestrum appears on MRI as an area of low signal intensity on both T1- and T2-weighted images due to its avascular nature. Surrounding granulation tissue, however, exhibits high signal intensity on T2-weighted images and enhances with contrast administration, highlighting the inflammatory response. PMC+3PMC+3PMC+3PMC+1PMC+1
In some cases, Computed Tomography (CT) scans provide detailed images of bone architecture, aiding in the identification of sequestra, especially when MRI is contraindicated. CT is particularly useful in surgical planning, offering precise localization of necrotic bone.
Advanced nuclear medicine techniques like Positron Emission Tomography (PET) and Single Photon Emission Computed Tomography (SPECT) can also be employed, especially in complex or recurrent cases, to assess metabolic activity and differentiate between active infection and other pathologies. PMC
Importance of Clinical History and Physical Examination
While imaging studies are invaluable, they must be interpreted in the context of a thorough clinical assessment. A detailed patient history, including prior infections, surgeries, trauma, or underlying conditions like diabetes, provides essential clues.
Physical examination may reveal signs such as:
- Localized pain and tenderness over the affected bone.
- Swelling and erythema, indicating inflammation.
- Sinus tract formation with purulent discharge, suggesting chronic infection.
- Reduced range of motion if the infection involves joints.
Laboratory investigations complement the clinical and imaging findings. Elevated inflammatory markers like Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP) support the diagnosis of osteomyelitis. Blood cultures, along with biopsy of the affected bone when possible, provide definitive identification of the causative organism, guiding targeted antibiotic therapy.
In summary, the diagnosis of a sequestrum is a multifaceted process that integrates clinical evaluation, imaging studies, and laboratory tests to ensure accurate identification and effective management.
Risk Factors That Increase Sequestrum Likelihood
Age and Immunocompromised Conditions
Certain populations are more susceptible to developing a sequestrum due to factors that impair bone healing and immune response.
Age plays a significant role:
- Children: The metaphyseal regions of long bones in children have a rich blood supply, making them prone to hematogenous spread of infection. However, their robust healing capacity often prevents progression to sequestrum if treated promptly.
- Elderly: Age-related vascular insufficiency and comorbidities like osteoporosis increase the risk of chronic osteomyelitis and sequestrum formation.
Immunocompromised states also elevate the risk:
- Diabetes Mellitus: Poor glycemic control impairs neutrophil function and blood flow, hindering infection resolution.
- Chronic Kidney Disease: Uremia affects immune competence, and dialysis patients are at increased risk due to frequent vascular access.
- HIV/AIDS: Immunodeficiency predisposes to atypical infections that can involve bone.
- Use of Immunosuppressive Therapy: Patients on corticosteroids or chemotherapy have diminished inflammatory responses, allowing infections to progress unchecked.
Surgical Complications and Poor Wound Healing
Postoperative infections are a significant concern, particularly in orthopedic procedures involving implants or prosthetics. Factors contributing to sequestrum formation include:
- Inadequate Sterilization: Contamination during surgery can introduce pathogens directly into bone tissue.
- Prolonged Surgical Time: Extended procedures increase exposure to potential contaminants.
- Poor Surgical Technique: Excessive periosteal stripping or thermal injury from drills can compromise bone vitality.
- Postoperative Hematoma: Accumulated blood serves as a medium for bacterial growth.
Additionally, patients with poor nutritional status, smoking habits, or peripheral vascular disease exhibit delayed wound healing, providing an opportunity for infections to establish and progress to chronic osteomyelitis with sequestrum formation.
Recognizing these risk factors allows for the implementation of preventive measures, such as optimizing glycemic control, ensuring sterile surgical environments, and promoting smoking cessation, to reduce the incidence of sequestrum.
Complications Associated with Untreated Sequestrum
Spread of Infection
A sequestrum acts as a nidus for persistent infection, shielded from immune surveillance and systemic antibiotics due to its avascular nature. If left untreated, the infection can extend beyond the bone, leading to:
- Soft Tissue Abscesses: Accumulation of pus in adjacent muscles or subcutaneous tissue.
- Sinus Tract Formation: Channels that drain purulent material to the skin surface, often chronic and difficult to heal.
- Septic Arthritis: Infection spreading into nearby joints, causing cartilage destruction.
- Systemic Sepsis: Bacteria entering the bloodstream, leading to widespread inflammatory response and potential organ failure.
These complications not only exacerbate patient morbidity but also complicate treatment, often necessitating more aggressive surgical interventions and prolonged antibiotic courses.
Osteomyelitis and Systemic Involvement
Chronic osteomyelitis resulting from an untreated sequestrum can lead to significant structural damage to the bone, including:
- Pathological Fractures: Weakened bone structure increases susceptibility to fractures with minimal trauma.
- Bone Deformities: Destruction and irregular healing can result in angular deformities, especially in growing children.
- Amyloidosis: Chronic inflammation may lead to amyloid protein deposition in organs, impairing their function.
- Squamous Cell Carcinoma: Long-standing sinus tracts have a rare risk of malignant transformation.
Early recognition and management of a sequestrum are crucial to prevent these severe outcomes. Multidisciplinary care involving infectious disease specialists, orthopedic surgeons, and rehabilitation teams ensures comprehensive treatment and reduces the risk of long-term complications.
Treatment Approaches for Sequestrum
Surgical Debridement and Sequestrectomy
When it comes to treating a sequestrum, surgery is usually unavoidable. Unlike infections in soft tissues that can often be managed with antibiotics alone, a sequestrum—being necrotic, avascular bone—serves as a persistent infection source that the body cannot eliminate on its own. The gold-standard procedure for removing this dead bone is known as a sequestrectomy.
Sequestrectomy involves surgically excising the dead bone fragment. This is typically accompanied by debridement, where surgeons also clean out any pus, granulation tissue, or other necrotic material surrounding the sequestrum. The goal is to create a clean, healthy bone bed that can heal and respond to antibiotic therapy.
The approach to surgery depends on the location and size of the sequestrum. For example:
- In long bones like the femur or tibia, the surgeon might make a cortical window to access and remove the necrotic fragment.
- In spinal or pelvic bones, where surgery is more complex, image-guided techniques or staged procedures might be used.
Surgery is often followed by bone grafting or flap coverage if a significant portion of bone or soft tissue is removed. This is particularly important to restore structural integrity and promote healing.
The timing of surgery is also crucial. In acute settings, it might be deferred until inflammation is controlled. In chronic cases, surgery is often scheduled after comprehensive imaging and lab work.
Antibiotic Therapy
While surgery removes the physical source of infection, antibiotics are essential to eliminate any residual bacteria and prevent recurrence. Treatment usually starts with broad-spectrum intravenous antibiotics, which may later be adjusted based on culture and sensitivity results.
Typical antibiotics used include:
- Vancomycin (for MRSA)
- Ceftriaxone or cefazolin (for MSSA)
- Clindamycin or Linezolid in penicillin-allergic patients
The duration of antibiotic treatment can vary:
- IV therapy for 4–6 weeks is standard.
- This may be followed by oral antibiotics for several additional weeks in chronic cases.
In some cases, local antibiotic delivery systems such as gentamicin beads or antibiotic-loaded spacers are used during surgery to provide high concentrations of antibiotics directly to the infected area.
Success hinges on a combined approach: surgical removal of the sequestrum, appropriate antimicrobial therapy, and ongoing monitoring.
Role of Imaging in Monitoring Progress
Post-Treatment Follow-Up
After treatment, whether surgical or conservative, imaging plays a pivotal role in ensuring that the infection has been completely eradicated and that healing is progressing appropriately. Post-treatment follow-up generally includes a combination of:
- X-rays to check for resolution of osteomyelitic changes and bone remodeling.
- MRI or CT scans if symptoms persist or recur.
- Ultrasound for evaluating soft tissue complications like abscesses.
Clinical symptoms should also be monitored. Pain reduction, absence of discharge, improved mobility, and normalization of inflammatory markers (like CRP and ESR) are positive signs.
Regular follow-up imaging helps in identifying:
- Recurrence of sequestrum
- Incomplete surgical removal
- Re-infection or new abscess formation
Preventing Recurrence with Imaging Insights
One of the key roles of imaging is preventing recurrence. If a small piece of sequestrum is left behind or if the infection begins to redevelop in nearby bone, early detection through imaging can make the difference between a quick reintervention and a prolonged battle with chronic infection.
MRI, in particular, offers the sensitivity to catch early marrow changes before symptoms even appear. In high-risk patients, regular imaging might be scheduled even in the absence of symptoms to ensure early intervention.
In some advanced centers, functional imaging techniques like PET scans are used to track metabolic activity and help distinguish between post-surgical changes and ongoing infection. This is particularly valuable in complex, multi-surgical cases or patients with compromised immune systems.
Alternative and Supportive Therapies
Pain Management Strategies
Dealing with sequestrum isn’t just about treating infection—it’s also about managing the chronic pain and discomfort that often accompany the condition. Bone infections are notorious for causing deep, aching pain that doesn’t always respond well to typical over-the-counter remedies.
Effective pain management involves:
- NSAIDs like ibuprofen or naproxen for inflammation and mild to moderate pain.
- Opioids for short-term use in severe pain scenarios.
- Neuropathic pain agents such as gabapentin or amitriptyline, especially if the infection has impacted surrounding nerves.
- Topical analgesics in cases with superficial sinus tracts.
In chronic cases, a multimodal pain management plan is often required, which might include physical therapy, psychological support, and interventional techniques like nerve blocks.
Physical Therapy and Rehabilitation
Recovery from sequestrum surgery or chronic osteomyelitis often involves a period of physical rehabilitation to restore function, strength, and mobility. This is especially important in cases where the infection affected weight-bearing bones like the femur or tibia.
Physical therapy may include:
- Range-of-motion exercises to prevent joint stiffness
- Strength training to rebuild muscle around the affected area
- Gait training in patients recovering from lower limb infections
- Occupational therapy if daily activities have been impacted
Rehabilitation is not just about physical health—it plays a key role in mental recovery as well. Chronic infections and long-term recovery can take a psychological toll. Support from rehabilitation specialists helps patients regain confidence and improve their quality of life.
Prognosis and Recovery Timeline
Factors Affecting Healing
The road to recovery from a sequestrum isn’t uniform—it varies depending on several factors:
- Extent of infection: Widespread osteomyelitis with multiple sequestra takes longer to heal than a localized lesion.
- Timeliness of treatment: Early intervention usually results in better outcomes.
- Patient health: Conditions like diabetes, smoking, and malnutrition delay healing.
- Surgical success: Complete removal of the sequestrum without damaging healthy bone is critical.
- Post-operative care: Adherence to antibiotics, proper wound care, and rehabilitation are essential for full recovery.
Long-Term Outlook for Patients
Most patients recover fully after appropriate surgical and medical treatment, especially when the infection is caught early. However, some may face long-term issues:
- Bone deformities
- Reduced mobility
- Chronic pain
- Recurrent infections
For these individuals, long-term monitoring and sometimes lifelong adjustments to lifestyle or medication are necessary. Still, with proper treatment, the prognosis is generally good, and many patients return to normal activities within several months.
Pediatric Considerations in Sequestrum Cases
Differences in Diagnosis and Treatment
Children are not just small adults, especially when it comes to bone infections like sequestrum. Their growing bones, unique blood supply, and developing immune systems mean that the diagnosis and management of sequestrum in pediatric cases require specialized approaches.
Diagnosis in children can be tricky. They may not communicate symptoms clearly, especially very young children who can’t articulate pain or discomfort. Instead, parents might notice:
- Limping or refusal to bear weight
- Crying when a limb is touched or moved
- Fever with no obvious source
- Swelling over a limb or joint
Pediatricians must maintain a high index of suspicion for osteomyelitis in any child with unexplained fever and localized pain. Early imaging is critical, and MRI is preferred for its superior soft tissue resolution without radiation exposure.
Treatment protocols for children also differ:
- Antibiotic dosing must be carefully adjusted for weight and age.
- Surgical intervention is approached with extra caution to avoid damaging growth plates.
- Minimally invasive techniques, such as percutaneous drainage, are often preferred.
In children, the bone can remodel over time, which often allows for better outcomes compared to adults. However, untreated or poorly managed infections can lead to:
- Growth disturbances
- Angular deformities
- Limb length discrepancies
These complications underscore the importance of timely intervention and ongoing monitoring throughout the growth period.
Special Care for Growing Bones
One of the most significant concerns in pediatric sequestrum is the potential damage to the epiphyseal (growth) plates. These areas are where new bone is formed, and any disruption can have lifelong consequences.
Special care must be taken during surgery to avoid:
- Cutting across the growth plate
- Excessive removal of bone that can compromise future growth
- Infections spreading to the joint space, especially in young children
Because children’s bones heal more rapidly, they may not always require extensive surgical intervention. However, this doesn’t mean the condition is less serious. Pediatric orthopedic specialists often follow these cases closely for months or even years to ensure that growth proceeds normally and complications are caught early.
Preventing Sequestrum Formation
Importance of Timely Treatment of Infections
The best treatment for sequestrum is prevention—and that starts with prompt recognition and treatment of bone infections before they progress to chronic osteomyelitis. In many cases, the opportunity to prevent a sequestrum is lost due to delays in diagnosis or suboptimal treatment of an early infection.
Here’s what prevention should look like:
- Early diagnosis of infections, especially in high-risk individuals like diabetics or post-operative patients.
- Immediate antibiotic therapy tailored to the suspected or confirmed pathogen.
- Drainage of abscesses or infected tissue, either surgically or through image-guided techniques.
- Close monitoring of patients recovering from orthopedic injuries or surgeries.
Timely management can often reverse early-stage osteomyelitis and prevent necrosis from setting in. The window of opportunity can be narrow—sometimes just days—so vigilance is key.
Proper Surgical Hygiene and Aftercare
Post-surgical sequestrum formation is a completely preventable complication in most cases. It boils down to sterile technique and diligent aftercare.
Key preventive strategies include:
- Maintaining aseptic conditions during all orthopedic procedures.
- Pre-operative screening for infection risks, such as MRSA colonization.
- Appropriate use of prophylactic antibiotics, especially for high-risk surgeries.
- Prompt wound care to detect and address early signs of infection.
Patient education is equally important. They should be taught to:
- Recognize signs of infection (redness, fever, swelling)
- Keep surgical sites clean and dry
- Follow up regularly with their healthcare provider
A minor lapse in hygiene or delay in follow-up care can be the difference between a clean recovery and the development of a chronic bone infection with sequestrum.
Sequestrum in Veterinary Medicine
Common in Horses and Dogs
Sequestrum isn’t just a human medical issue—it affects animals too, particularly horses and dogs, due to their high risk of trauma and infections. In equine medicine, it’s quite common because horses often sustain injuries to their limbs that go unnoticed or untreated.
In dogs, sequestrum usually follows bone trauma, surgery, or bite wounds. Breeds that are particularly active or prone to joint issues—like German Shepherds or Labradors—are more likely to develop it.
Signs in animals include:
- Persistent lameness
- Swelling at the site of a previous injury
- Discharge from the skin
- Pain upon palpation
Veterinarians use similar diagnostic tools—X-rays, MRI, and sometimes bone scans—to identify sequestra in animals. The treatment often involves surgical removal, followed by a course of antibiotics and careful monitoring.
Diagnostic and Surgical Differences
In veterinary practice, diagnosing a sequestrum can be more complex because animals cannot express pain verbally. Vets rely heavily on observation, owner reports, and palpation. Advanced imaging like MRI is less frequently used due to cost and availability, especially in large animals.
Surgical treatment also has its challenges:
- General anesthesia carries higher risks in certain breeds or older animals.
- Post-surgical care requires careful management, especially with animals prone to biting, licking, or reopening wounds.
- Re-infection risks are high if the wound is not kept clean.
Despite these hurdles, modern veterinary medicine has made significant strides. With timely care, most animals recover fully after sequestrum removal.
Latest Research and Developments
Innovations in Bone Healing
Research in bone regeneration and infection control is rapidly evolving, offering new hope for patients suffering from chronic infections and sequestrum. Some exciting innovations include:
- Bioengineered bone grafts that incorporate antibacterial agents
- 3D-printed bone scaffolds that can replace large areas of necrotic bone
- Antibiotic-loaded nanoparticles that penetrate deeper into infected tissues
- Bone-seeking antibiotics that target the sequestrum directly
Stem cell therapy is another area showing promise. Studies are underway to evaluate whether mesenchymal stem cells can help regenerate bone and modulate immune responses in osteomyelitis.
Future of Sequestrum Treatment
In the future, we might see a shift from invasive surgeries to minimally invasive or regenerative therapies. The integration of AI in imaging is helping clinicians detect sequestrum earlier and plan surgeries more precisely.
Some other breakthroughs on the horizon:
- Biodegradable implants that slowly release antibiotics
- Smart wound dressings that change color in the presence of infection
- Gene editing techniques to enhance bone immunity and resistance to infection
As these technologies become more widely available, we can expect to see faster recovery times, fewer complications, and a dramatic reduction in chronic cases.
Conclusion
Sequestrum, though a small fragment of dead bone, carries enormous clinical significance. It often signals the chronicity of an infection, requiring not just medical intervention but a carefully coordinated surgical and rehabilitative approach. From initial diagnosis to long-term recovery, managing sequestrum demands vigilance, precision, and teamwork among healthcare professionals.
With advances in imaging, surgical techniques, and regenerative medicine, outcomes have improved significantly. But prevention remains the most powerful tool—timely treatment of infections, meticulous surgical practices, and patient education are the keys to keeping this complication at bay.
If you or someone you know is facing a potential bone infection, don’t delay. Seek medical advice immediately. Because when it comes to sequestrum, early action is everything.
FAQs
1. Can sequestrum go away on its own?
No, a sequestrum cannot be reabsorbed or healed naturally by the body. It usually requires surgical removal, as the dead bone has no blood supply and can harbor bacteria indefinitely.
2. How long does it take to recover from sequestrum surgery?
Recovery time varies but generally ranges from 6 to 12 weeks. It depends on the extent of surgery, location of the sequestrum, and overall patient health.
3. What are the chances of recurrence?
Recurrence is possible, especially if the sequestrum was not completely removed or if the underlying infection was not fully treated. Proper follow-up care and antibiotics reduce this risk.
4. Is sequestrum life-threatening?
While the sequestrum itself isn’t immediately life-threatening, the infection it harbors can spread, leading to systemic issues like sepsis, which can be fatal if untreated.
5. What type of doctor treats sequestrum?
An orthopedic surgeon typically handles sequestrum cases, often working alongside infectious disease specialists for comprehensive care.