What is Myelomalacia?
Myelomalacia is a serious neurological condition involving the softening of the spinal cord. This degeneration of the spinal cord tissue typically results from a loss of blood supply (ischemia), physical trauma, or prolonged compression due to spinal issues like herniated discs or spinal stenosis. The term itself originates from the Greek words “myelo,” meaning “spinal cord,” and “malakia,” meaning “softening.” This softening disrupts the normal architecture of the spinal cord, which leads to permanent nerve damage.
Unfortunately, myelomalacia is progressive in nature if left untreated, which makes early detection and intervention essential. While it is not always possible to reverse the damage once it has occurred, timely treatment can prevent further deterioration and significantly improve the patient’s quality of life.
Difference Between Myelomalacia and Myelopathy
These two terms are often confused, but they refer to different aspects of spinal cord issues. Myelomalacia describes the physical and pathological degeneration (i.e., softening) of spinal cord tissue. In contrast, myelopathy refers to the clinical manifestation of spinal cord dysfunction, essentially, the symptoms that arise when the spinal cord isn’t working properly.
Think of myelopathy as the outward signs (like weakness, numbness, poor coordination), while myelomalacia is the internal damage seen on imaging like MRI scans. You can have myelopathy without myelomalacia if the cord is compressed but not yet softened. But once the tissue starts to degenerate, you’re likely dealing with both conditions, and the situation becomes more serious.
Myelopathy might be managed with conservative measures, but myelomalacia usually requires urgent intervention to prevent permanent damage.
Anatomy of the Spinal Cord
The spinal cord is a long, cylindrical structure composed of nervous tissue and protected by the vertebral column. It extends from the brainstem down to the lower back and functions as the primary communication between the brain and body. The spinal cord is divided into four main regions: cervical, thoracic, lumbar, and sacral.
Inside the spinal cord, white matter surrounds a central area of gray matter. The white matter contains nerve fibers that transmit messages up to the brain (sensory pathways) and down to the body (motor pathways). Any disruption in this communication system, like what occurs in myelomalacia, can severely impact bodily functions.
The spinal cord is surrounded by cerebrospinal fluid, which cushions it, and it’s protected by vertebrae and meninges. Blood vessels run along its surface, supplying the necessary nutrients and oxygen. When these blood vessels are compromised, due to injury, inflammation, or disease, it can cause the spinal cord tissue to become ischemic and begin to soften.
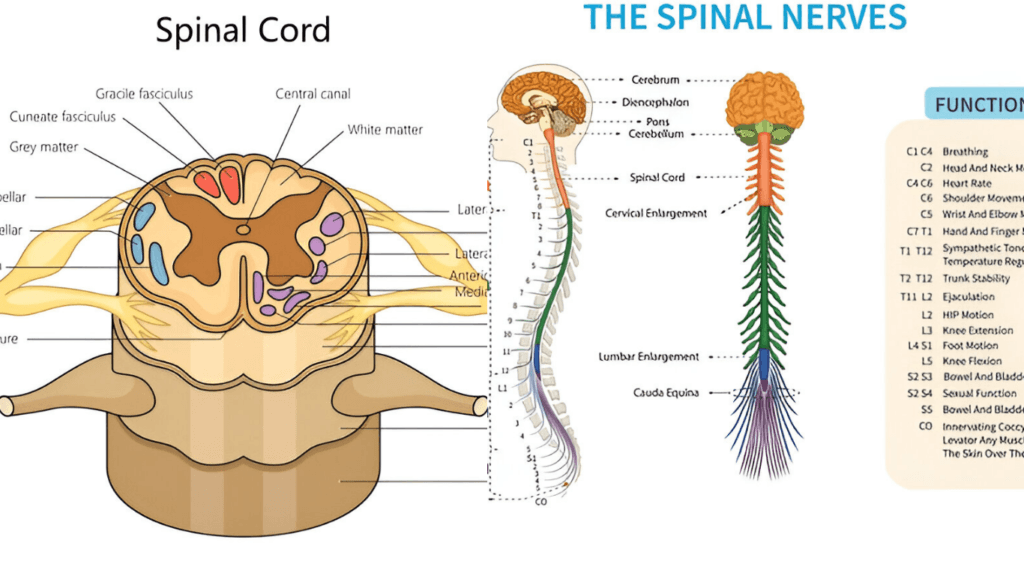
Function of the Cervical Cord
The cervical spinal cord is located in the neck and consists of eight segments (C1 to C8). It is responsible for sending nerve signals to and from the brain that control the head, neck, diaphragm (for breathing), shoulders, arms, and hands. This makes it an incredibly vital region of the spinal cord.
Damage to the cervical cord can lead to devastating consequences. For example, injuries at or above C3 can result in respiratory failure because the diaphragm is no longer properly innervated. Lower cervical cord damage (C5–C8) can result in arm and hand weakness or paralysis, as well as impaired fine motor control.
Because of its location and critical functions, cervical myelomalacia is considered more dangerous than when the condition occurs lower in the spinal cord. Even minor damage in this region can lead to significant disability or life-threatening complications.
Importance of Spinal Cord Health
A healthy spinal cord allows for efficient communication between the brain and the rest of the body. It controls both voluntary movements (like walking or writing) and involuntary actions (like heart rate, digestion, and breathing).
When spinal cord health is compromised, it can result in a cascade of problems, including muscle weakness, sensory loss, balance issues, and even problems with bladder and bowel control. Conditions like myelomalacia, spinal cord infarction, and chronic spinal compression demonstrate just how fragile and essential this structure is.
Protecting spinal cord health involves maintaining good posture, staying physically active with low-impact exercises, managing chronic conditions like diabetes or arthritis, and seeking immediate care for any spinal injuries. Preventative care, such as regular medical checkups and prompt attention to neurological symptoms, plays a key role in avoiding irreversible damage.
Causes of Myelomalacia
Common Causes:
Trauma is one of the leading causes of myelomalacia. Car accidents, falls, sports injuries, or any other incidents that result in spinal fractures or dislocations can disrupt the blood flow to the spinal cord, leading to softening and degeneration.
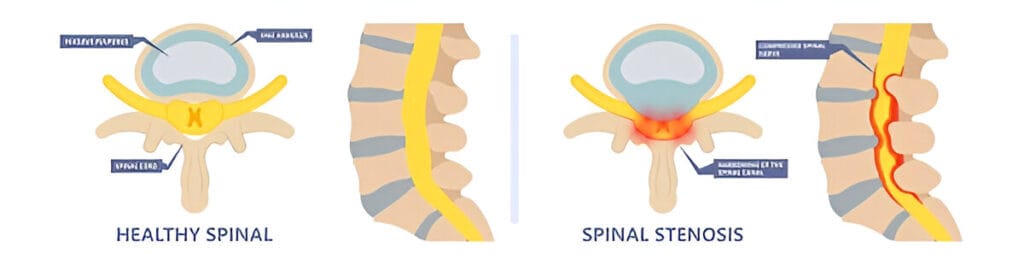
Herniated discs are another frequent culprit. When a spinal disc bulges or ruptures, it can press against the spinal cord, reducing blood flow and causing inflammation. Over time, this chronic compression can result in myelomalacia, particularly if not treated.
Degenerative diseases like osteoarthritis and spinal stenosis also play a major role. These conditions cause a gradual narrowing of the spinal canal, putting persistent pressure on the spinal cord. In older adults, this is one of the most common pathways to developing myelomalacia.
Spinal Cord Infarction and Its Role
Spinal cord infarction refers to the loss of blood supply to the spinal cord—essentially, a stroke of the spine. Just like a brain stroke, this cuts off oxygen and nutrients, leading to tissue death. If the affected area doesn’t receive blood flow quickly, the damage becomes permanent and can result in myelomalacia.
Infarctions often occur due to atherosclerosis (hardening of arteries), blood clots, or trauma. The signs can appear suddenly—sudden weakness, numbness, or loss of function below the level of infarction. Without immediate medical intervention, the spinal cord may begin to soften and deteriorate.
Inflammatory and Autoimmune Triggers
Some cases of myelomalacia are linked to chronic inflammation or autoimmune diseases. Conditions like multiple sclerosis, lupus, and neuromyelitis optica can cause immune system attacks on the spinal cord. This inflammation disrupts blood supply and damages tissue over time.
Chronic inflammation, even from untreated infections like spinal tuberculosis or syphilis, can also contribute. These cases are less common but especially dangerous because symptoms may progress silently until significant damage has occurred.
Symptoms of Myelomalacia
Early Symptoms:
- Tingling sensations,
- Numbness or weakness in the arms or legs. This may start as a loss of grip strength, difficulty with fine motor skills (like writing), or stumbling while walking.
These symptoms often progress slowly and are sometimes mistaken for more common conditions like carpal tunnel syndrome or peripheral neuropathy. However, unlike these peripheral issues, myelomalacia originates in the central nervous system, making it far more serious.
Left unchecked, symptoms can quickly worsen, leading to more debilitating issues.
Progression of Symptoms Over Time
- Weakness spreads from one limb to multiple, balance worsens, and muscle spasms or involuntary jerking may appear.
- Patients may also experience chronic pain, hypersensitivity, or a burning sensation in affected areas.
- Eventually, this leads to partial or complete loss of motor control below the level of the spinal cord lesion.
- In advanced cases, patients may lose bladder and bowel control, suffer from constant pain, or develop breathing difficulties if the cervical spine is involved.
The progression can be slow or rapid, depending on the cause. Regular monitoring is essential to assess changes and modify treatment accordingly.
Cervical Myelomalacia Symptoms vs. General Myelomalacia Symptoms
When the softening occurs in the cervical spine, symptoms tend to be more dramatic and widespread. Cervical myelomalacia often causes:
- Weakness in the arms and hands
- Poor coordination
- Neck stiffness or pain
- Difficulty breathing or swallowing
- Bladder dysfunction
General myelomalacia (in thoracic or lumbar regions) may present with more localized symptoms like:
- Leg weakness
- Gait abnormalities
- Loss of reflexes
- Back pain or numbness
Because the cervical spine is so close to the brain and houses nerves that control upper body and diaphragm, cervical cases are typically more urgent and potentially life-threatening.
Related: Cervical Myelopathy Recovery Time
Myelomalacia Diagnosis: MRI, Tests & Early Detection
Importance of Early Diagnosis
Diagnosing myelomalacia early can make all the difference. Since it’s a progressive condition, the sooner it’s identified, the better the chances of preventing permanent damage. Unfortunately, early symptoms are often vague and misdiagnosed.
If you’re experiencing unusual weakness, numbness, or coordination problems—especially after a spinal injury—it’s vital to see a neurologist. Early diagnosis not only improves treatment success but may also prevent costly surgeries or lifelong disability.
MRI Imaging and What It Reveals
Magnetic Resonance Imaging (MRI) is the gold standard for diagnosing myelomalacia. MRI scans offer detailed images of the spinal cord and surrounding structures, allowing doctors to detect:
- T2 hyperintensity (a sign of softening or edema)
- Cord compression
- Loss of spinal cord volume
- Abnormal signal changes
Radiologists often look for signs like “spinal cord signal abnormality,” which usually indicates chronic damage. MRI also helps differentiate myelomalacia from other conditions like tumors, infections, or syringomyelia.
Other Diagnostic Tools: Physical Exams and Neurological Tests
Besides imaging, physical and neurological exams are crucial. Doctors assess:
- Reflexes
- Muscle strength
- Sensation response
- Coordination
- Gait and balance
Electromyography (EMG) and nerve conduction studies might also be used to rule out peripheral nerve disorders. These tests help confirm that the symptoms are originating in the spinal cord rather than from muscle or peripheral nerve damage.
Cervical Myelomalacia Treatment Approaches
- Non-Surgical Treatments
If caught early, non-surgical management may include physical therapy, pain management strategies, and bracing to reduce neck movement. Lifestyle changes like improving posture, avoiding high-impact activities, and weight management can reduce spinal pressure and inflammation. - When is Surgery Necessary?
Surgery becomes necessary when symptoms worsen or MRI shows progressive spinal cord damage. Decompression surgery can prevent further deterioration. Cervical fusion might be performed to stabilize the spine post-decompression. The goal is always to protect the remaining spinal cord function and prevent further myelomalacia progression. - Post-Surgical Recovery
Recovery involves a mix of physical therapy, occupational therapy, and ongoing monitoring. Some patients regain lost function, while others may only see symptom stabilization. It’s essential to set realistic expectations and remain consistent with rehab efforts. Long-term recovery often hinges on early intervention and a patient’s commitment to follow-through.
How to Prevent Further Spinal Cord Damage
- Early Detection is Key
The sooner spinal cord damage is identified, the better the outcome. That’s why symptoms like tingling, numbness, and weakness should never be ignored. Annual spinal health checkups and quick MRI diagnostics are recommended for those with chronic back or neck pain, especially after injuries. - Spinal Cord Health Tips
Maintaining good spinal health involves a holistic approach:- Exercise regularly to strengthen core and back muscles.
- Practice good posture—especially when sitting at desks or using devices.
- Avoid carrying heavy loads improperly.
- Eat an anti-inflammatory diet rich in omega-3s, leafy greens, and lean proteins.
- Quit smoking and limit alcohol, both interfere with spinal circulation and healing.
- Use of Assistive Devices
In some cases, braces or walking aids help reduce strain on the spine. These tools prevent falls, reduce pain, and improve mobility. Your doctor or physical therapist can recommend specific devices that best support your needs.
Myelomalacia in Different Age Groups
- In Younger Adults
Although rare, younger individuals can develop myelomalacia due to sports injuries, extreme trauma, or congenital abnormalities. Early intervention in this group often results in better outcomes due to stronger regenerative potential and quicker healing responses. - In Middle-Aged and Older Adults
For those over 40, degenerative disc disease and spinal stenosis become primary culprits. Symptoms may be misdiagnosed as arthritis or aging-related decline. This demographic must advocate for proper imaging and specialist referrals when neurological symptoms are present. - Children and Adolescents
Extremely rare but possible, pediatric myelomalacia can occur due to spinal cord malformations or birth trauma. Treatment is typically surgical, and outcomes vary widely depending on the underlying cause and timing of diagnosis.
Lifestyle Tips for Managing Myelomalacia Long-Term
- Healthy Living Matters
When you’re managing a condition like myelomalacia, every choice you make in your daily life can influence your spinal health. Leading a healthy lifestyle isn’t just a recommendation—it’s a necessity. A diet rich in anti-inflammatory foods like berries, leafy greens, salmon, turmeric, and walnuts can help reduce inflammation and support nerve health. Hydration is equally essential to keep spinal discs well-lubricated and functioning. - Exercise the Right Way
Physical activity is still important, but you need to adapt your routine. Gentle, low-impact exercises like swimming, walking, and stretching can keep your spine flexible and your muscles strong without straining your spinal cord. Always avoid activities that involve heavy lifting or jerky motions that can worsen cord compression. - Prioritize Mental Health
Chronic neurological conditions often take a toll on mental health. It’s easy to feel isolated or overwhelmed, but counseling, mindfulness practices, and support groups can make a huge difference. Talking to others going through similar experiences helps normalize the struggle and provides fresh coping strategies.
Prognosis and Long-Term Outlook for Myelomalacia Patients
- Can myelomalacia be reversed?
“While myelomalacia damage is usually permanent, early treatment (surgery, therapy) can halt progression and improve quality of life. Learn more about recovery timelines.”- Quality of Life Considerations
A lot depends on how early the condition is caught and the patient’s overall health. Some may experience only mild weakness, while others could require assistive devices for mobility. But with today’s medical advancements and increasing awareness, many live comfortably with appropriate care.- Ongoing Monitoring
Routine follow-ups are essential. Regular MRIs, neurological exams, and functional assessments help ensure the condition remains stable. If symptoms start returning or worsening, immediate reevaluation is critical to avoid further spinal cord damage.
Common Misconceptions About Myelomalacia
- “It’s Just a Back Problem”
Myelomalacia is far more than back pain. It’s a serious neurological condition that can affect everything from mobility to bladder control. Mistaking it for a simple orthopedic issue can delay life-saving treatment. - “Surgery Will Fix Everything”
While surgery can stop progression, it often cannot reverse damage already done. That’s why early intervention is so important. Surgery is just one part of a comprehensive treatment plan. - “It Only Affects Old People”
Although more common with age due to spinal degeneration, myelomalacia can affect people of all ages, especially those with spinal injuries or underlying neurological conditions.
When to Seek Immediate Medical Help
- Red Flag Symptoms
If you’re experiencing sudden loss of strength, increasing numbness, difficulty breathing, or bladder and bowel control issues—don’t wait. These are signs that the spinal cord may be rapidly deteriorating. - Who to See
Your first stop should be a neurologist or spine specialist. They can order the necessary imaging and guide you through a treatment plan. Avoid ignoring symptoms or relying solely on primary care—myelomalacia requires specialized knowledge.
Conclusion:
Myelomalacia is not something to take lightly. While it might start with subtle symptoms like tingling or weakness, it can quickly progress into a life-altering condition if ignored. Thankfully, modern medicine offers a range of diagnostic tools and treatments that can manage and even halt its progression. The key is awareness. Recognize the signs, push for a diagnosis, and commit to a treatment and lifestyle plan. Your spinal cord is the communication highway of your body—take care of it like your life depends on it, because in many ways, it truly does.
FAQs
1. Can myelomalacia go away on its own?
No, myelomalacia does not resolve without treatment. It typically requires medical or surgical intervention to halt its progression.
2. What does myelomalacia feel like?
Patients often describe it as a combination of numbness, tingling, weakness, and sometimes pain or burning sensations in the limbs.
3. Is myelomalacia fatal?
It’s not typically fatal, but in severe cervical cases, it can affect breathing or other critical functions, which can become life-threatening.
4. How fast does myelomalacia progress?
Progression varies. Some patients worsen over months, others over years. Timely diagnosis and treatment greatly influence the pace and outcome.
5. What kind of doctor treats myelomalacia?
Neurologists, spine surgeons, and orthopedic spine specialists are the primary experts in diagnosing and treating myelomalacia.