Joint injuries sneak up on office workers, construction crews, seniors, and even weekend warriors. From wrist pain to serious spinal trauma, joint injuries cover a wide spectrum of conditions that can affect mobility, productivity, and quality of life. But what exactly qualifies as a joint injury?
What Are Joint Injuries?
A joint is where two or more bones meet, and it’s supported by various soft tissues that allow smooth movement while maintaining stability. A joint injury typically involves damage to one or more parts of a joint—this could be the bones that meet, the cartilage that cushions them, or the ligaments, tendons, and discs that provide structure and movement.
Joint injuries can be categorized in two primary ways: traumatic injuries and overuse injuries.
Traumatic Injuries
These occur suddenly, often due to external force or impact. Falls, car accidents, or sports collisions can lead to fractures, dislocations, or acute ligament tears. For example, a sudden twist while running could result in a torn ACL or an ankle sprain.
Overuse Injuries
These injuries develop gradually over time. They’re caused by repetitive motion or chronic stress on a joint without adequate rest or conditioning. Carpal tunnel syndrome, for instance, is a textbook overuse injury resulting from repetitive wrist movements like typing or using tools.
Cervical Disc Herniation
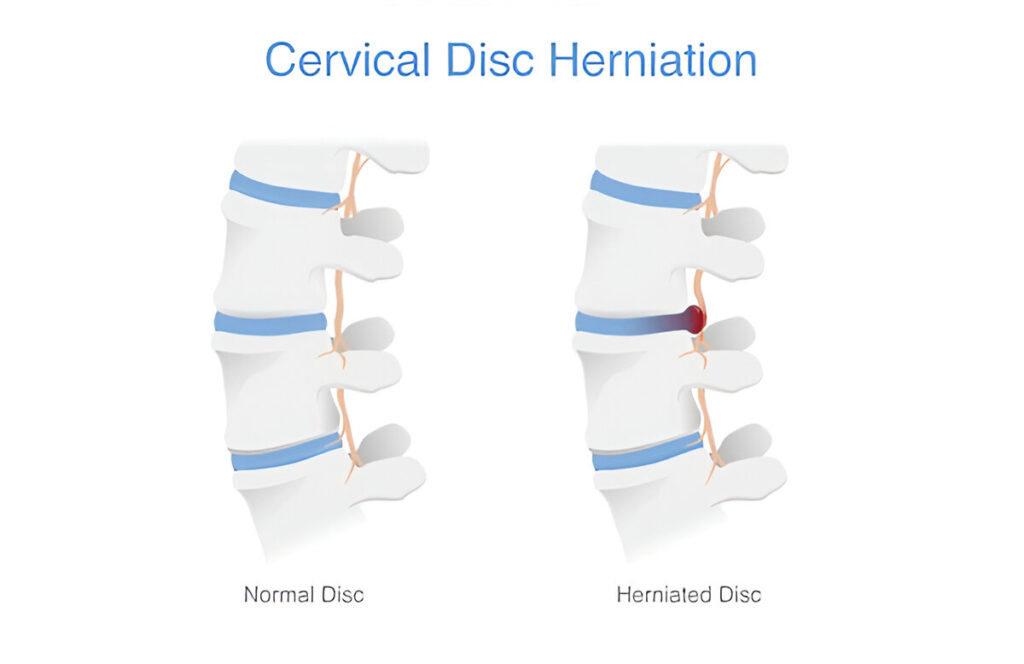
A cervical disc herniation happens when one of the discs in your neck (usually between vertebrae C4–C7) becomes damaged and the soft, jelly-like center bulges or leaks out. This can irritate nearby nerves, causing pain not just in the neck but also in the shoulders, arms, and even fingers.
Causes
- Trauma: Sudden impacts, such as car accidents or falls
- Aging: As discs degenerate, they become more prone to herniation
- Repetitive Strain: Poor posture or repetitive neck motion over time
Symptoms
- Sharp or burning neck pain
- Radiating pain into the arm or shoulder
- Numbness or tingling
- Muscle weakness in the arms
- Headaches, especially at the base of the skull
Diagnosis
Your doctor will typically start with a physical exam and review of symptoms. To confirm the diagnosis, imaging tests like MRI or X-rays are used to pinpoint the herniated disc and check for nerve compression.
Treatment Options
- Rest and activity modification
- Physical therapy to strengthen neck muscles and improve posture
- Steroid injections to reduce inflammation
- Surgery (like anterior cervical discectomy and fusion) in severe cases
For a deep dive into treatments and recovery timelines, check out our internal guide: [Cervical Disc Herniation Treatment & Recovery] (coming soon).
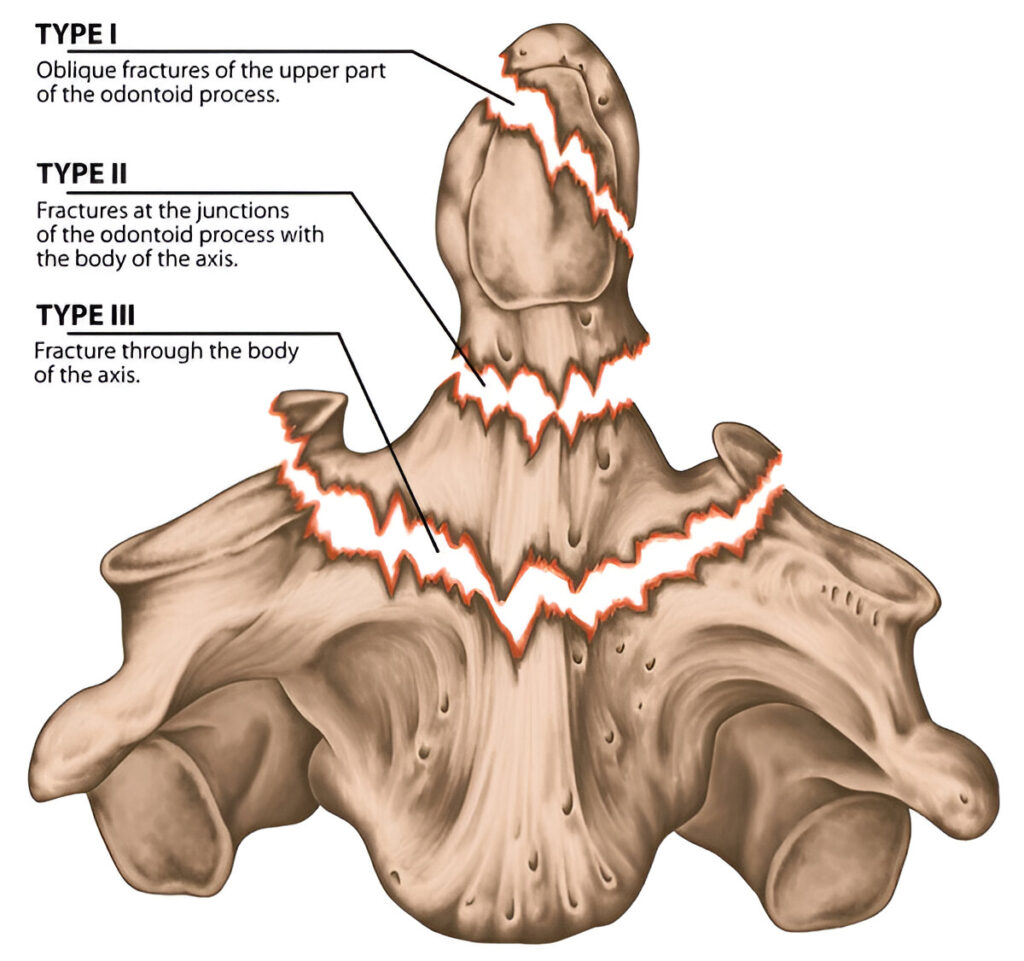
Odontoid Fractures (C2 Vertebral Fracture)
The odontoid fracture occurs at the C2 vertebra, specifically at the dens (a peg-like projection that allows your head to rotate). It’s dangerous due to its proximity to the brainstem and spinal cord. Elderly adults and High-velocity trauma victims, such as car or motorcycle accidents, are at high risk.
Symptoms
- Severe neck pain
- Difficulty moving the neck
- Neurological symptoms: numbness, weakness, or unsteadiness
- In some cases, the only symptom may be neck stiffness
Diagnosis
Imaging is crucial. CT scans provide a detailed view of the fracture, while MRIs can detect spinal cord involvement or soft tissue damage.
Treatment Options
- Cervical collar: For stable fractures, especially in older patients
- Halo brace: External fixation used in more complex or unstable cases
- Surgical fusion: Required if the fracture is displaced or not healing properly
This isn’t a “wait and see” injury. Prompt diagnosis and management are vital to prevent permanent damage. Learn more in our future article: Odontoid Fracture Types & Management.
Ankle Sprains
A sprained ankle is a sudden twist, an awkward step, or landing wrong during a jump can all stretch or tear the ligaments that stabilize your ankle. The most frequently injured ligament is the anterior talofibular ligament (ATFL).

Common Causes
- Sports that involve jumping or lateral movements (basketball, tennis)
- Walking on uneven terrain
- Wearing unstable footwear
Symptoms
- Pain, especially on the outer side of the ankle
- Swelling and bruising
- Difficulty putting weight on the foot
- Limited range of motion
Sprain Grades
- Grade I – Mild stretching of ligaments, slight swelling
- Grade II – Partial tear, moderate swelling, some instability
- Grade III – Complete tear, severe swelling, joint instability
Treatment – Think R.I.C.E.
- Rest: Keep weight off the injury
- Ice: Reduce swelling
- Compression: Use an elastic bandage
- Elevation: Raise the foot to reduce fluid buildup
Carpal Tunnel Syndrome
Carpal Tunnel Syndrome (CTS) develops gradually. This condition occurs when the median nerve is compressed as it passes through the carpal tunnel in your wrist. It’s especially common in people who perform repetitive hand movements, like typing or using tools.

Causes
- Repetitive wrist motion (typing, assembly line work)
- Wrist arthritis or trauma (e.g., fractures)
- Fluid retention (common during pregnancy)
- Diabetes or thyroid disorders
- Poor ergonomics at a workstation
Symptoms
- Numbness or tingling in the thumb, index, and middle fingers
- Pain that wakes you at night
- Weakness in the hand, especially difficulty gripping objects
- A feeling that your hand is “falling asleep” frequently
Many people initially ignore the symptoms, attributing them to fatigue. But untreated CTS can lead to permanent nerve damage and muscle atrophy.
Diagnosis
Diagnosis is usually clinical, supported by physical tests:
- Tinel’s Sign: Tapping the wrist causes tingling
- Phalen’s Test: Flexing the wrist intensifies symptoms
- Electromyography (EMG) or Nerve Conduction Studies: Measure electrical activity in the nerve
Treatment Options
- Wrist splints, especially at night
- Ergonomic adjustments (keyboard position, posture)
- Steroid injections to reduce inflammation
- Surgical release of the carpal tunnel in severe or unresponsive cases
Read more in our article: Carpal Tunnel Syndrome: Symptoms, Treatment & Prevention (coming soon).
ACL Tears
Anterior Cruciate Ligament (ACL) tears are one of the most feared injuries in sports. This ligament runs diagonally across the middle of the knee and is essential for stabilizing the joint during sudden stops or directional changes.
- Causes: Pivoting motions in sports like soccer, basketball, and skiing
- Symptoms: A popping sound at the time of injury, followed by swelling, instability, and pain
- Treatment: Ranges from rest and physical therapy to surgical reconstruction in severe cases
Shoulder Dislocations
The shoulder joint is the most mobile joint in the body—which also makes it highly susceptible to dislocation. This occurs when the upper arm bone pops out of the shoulder socket.
- Causes: Trauma from falls, contact sports, or accidents
- Symptoms: Visible deformity, intense pain, inability to move the arm
- Treatment: Reduction (putting the shoulder back in place), followed by rest and physical therapy; recurrent dislocations may require surgery
Compression Fractures
These are spinal fractures, most commonly seen in the thoracic or lumbar vertebrae, often caused by osteoporosis or trauma.
- Causes: Falls, car accidents, or even minor stress in weakened bones
- Symptoms: Sudden back pain, height loss, stooped posture
- Treatment: Pain management, bracing, physical therapy, and in severe cases, procedures like vertebroplasty or spinal fusion
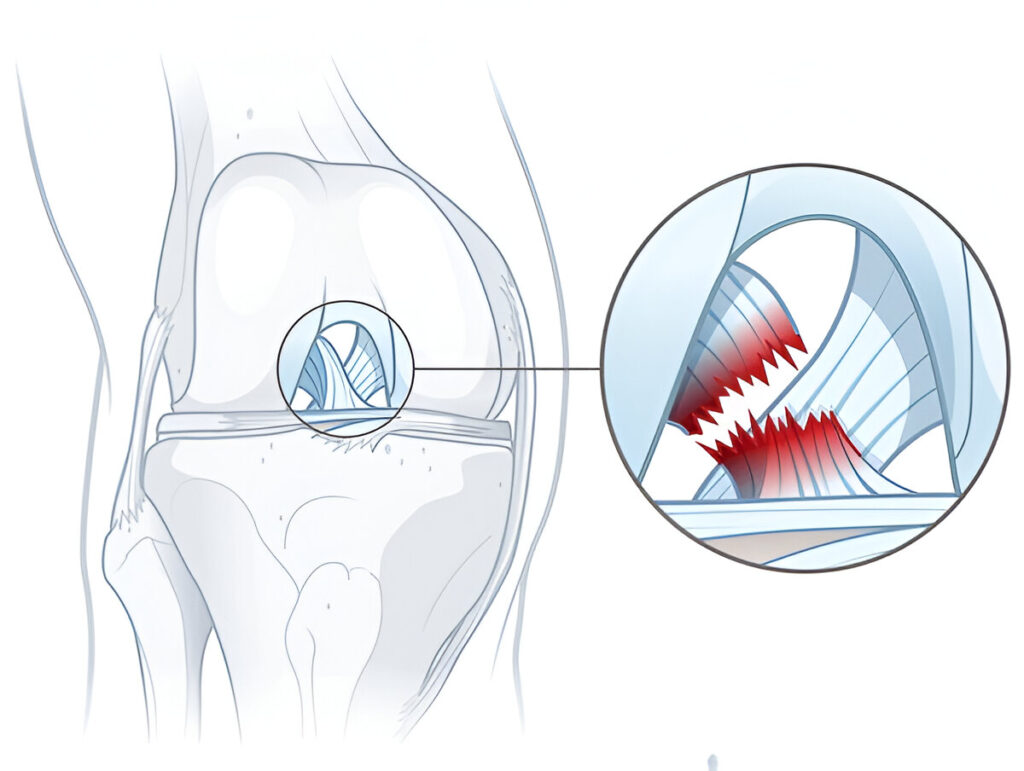
Meniscus Tears
Your meniscus is the cartilage in your knee that cushions and stabilizes the joint. Tears are common in athletes and older adults with degenerative joint changes.
- Causes: Twisting or rotating the knee while bearing weight
- Symptoms: Pain, swelling, stiffness, clicking or locking of the knee
- Treatment: Ranges from conservative (RICE, PT) to surgical repair or partial meniscectomy
Plantar Fasciitis
While not a joint injury in the strictest sense, plantar fasciitis affects the connective tissue that supports the arch of your foot and is a major cause of heel pain.
- Causes: Overuse, poor footwear, flat feet, high arches
- Symptoms: Sharp pain in the heel, especially with the first steps in the morning
- Treatment: Stretching, orthotic insoles, physical therapy, night splints, and corticosteroid injections
Wrist Fractures
A wrist fracture typically involves the distal radius and is very common when people try to break a fall with an outstretched hand.
- Causes: Falls, sports injuries, car accidents
- Symptoms: Swelling, bruising, pain, deformity, difficulty gripping
- Treatment: Immobilization with a cast or splint; severe cases may require surgery with pins, plates, or screws
When to See a Doctor
Joint injuries are common, but not all require medical intervention. However, ignoring serious signs can lead to long-term damage or even permanent disability. So, how do you know when it’s time to stop Googling and start dialing your doctor?
Red Flags You Shouldn’t Ignore
- Persistent pain that doesn’t improve with rest or over-the-counter meds
- Swelling that lasts more than a few days or worsens over time
- Inability to move the joint or bear weight on it
- Visible deformities, like crooked fingers or an angled limb
- Numbness or tingling, especially if it spreads
- Instability—if your joint feels like it might give out
In Emergencies
- Severe trauma, such as from a car crash or a fall from height
- Sudden loss of movement or sensation
- Signs of infection, like redness, warmth, fever, or pus near a joint
Don’t “tough it out” or assume the injury will heal on its own. Early diagnosis can drastically improve recovery and prevent complications like chronic pain or arthritis.
If in doubt, consult an orthopedic specialist or visit an urgent care center. Peace of mind is worth it—so is avoiding long-term damage.
Recovery & Long-Term Joint Care
Recovery doesn’t stop when the swelling goes down. Joint injuries often require weeks—or even months—of rehab, especially if tendons, ligaments, or spinal components are involved. Long-term joint care ensures you heal correctly and reduce the risk of future problems.
Physiotherapy Is Key
A structured physical therapy program helps rebuild strength, restore mobility, and prevent stiffness. Depending on your injury, therapy may include:
- Stretching and mobility exercises
- Resistance training
- Balance and proprioception work
- Manual therapy (massage, joint mobilization)
Missing this step or “half-doing” your rehab is one of the fastest ways to end up with chronic joint issues or reinjury.
Supplements and Nutrition
Your joints need more than movement—they need nutritional support, too:
- Glucosamine & Chondroitin: Often used for cartilage support
- Omega-3 fatty acids: Reduce inflammation
- Vitamin D & Calcium: Crucial for bone and joint health
- Collagen: May help improve joint flexibility and healing
Joint-Friendly Lifestyle Tips
- Stay active: Low-impact exercises like swimming or cycling help maintain joint health
- Manage weight: Less weight = less stress on joints
- Listen to your body: Don’t push through joint pain
- Regular checkups: Monitor healing progress, especially for spinal or complex joint injuries
Recovery isn’t just about getting back to “normal”—it’s about building a new, stronger baseline for the future.
Preventing Joint Injuries
An ounce of prevention is worth a pound of cure, especially when it comes to joint health. Whether you’re an athlete, office worker, or senior citizen, protecting your joints is essential for long-term mobility and quality of life.
Warm-Up and Conditioning
- Always warm up before exercise or physical activity
- Focus on dynamic stretches and mobility drills
- Strengthen supporting muscles (e.g., quads, core, shoulders)
Posture & Body Mechanics
- Lift with your legs, not your back
- Keep your spine neutral during tasks
- Don’t hyperextend joints during exercise or daily movements
Workplace Ergonomics
- Adjust your keyboard and monitor height
- Use wrist supports if typing for long hours
- Take frequent breaks to stretch and move
Special Tips for Older Adults
- Install non-slip mats and handrails
- Engage in balance training like Tai Chi or yoga
- Get regular bone density screenings to catch osteoporosis early
Small daily changes can make a massive difference in joint longevity. Think of your joints like car tires—rotate, balance, and align them regularly to avoid breakdowns!
Final Thoughts
Joint injuries might be common, but they’re far from trivial. Whether it’s a twisted ankle on a morning jog or a serious spinal injury from a fall, every joint issue deserves attention and care.
Early diagnosis, prompt treatment, and consistent rehab aren’t just helpful—they’re critical. Don’t fall into the trap of pushing through pain or self-diagnosing your symptoms. You only get one body—treat it well, and it’ll return the favor.
Spread awareness, encourage your loved ones to be mindful of their joint health, and never ignore the signals your body sends. Whether you’re bouncing back from an injury or simply trying to stay pain-free, knowledge is your strongest tool.
FAQs
How long does a cervical disc herniation take to heal?
Can carpal tunnel be reversed without surgery?
What’s the difference between a sprain and a fracture?
Is an odontoid fracture life-threatening?
When should you see an orthopedic specialist for joint pain?
Pain persists for more than a few weeks
You notice swelling, instability, or limited range of motion
You experience frequent or recurring injuries
Over-the-counter pain medications or home remedies aren’t effective
There are signs of nerve involvement like numbness, tingling, or weakness
Early evaluation helps in preventing complications and ensures you’re on the right treatment path, whether it’s physical therapy, imaging, or surgical options.