“Is it just aging—or something more?”
If you’re over 50 and wondering why your formerly smooth moves now come with aches and stiffness. Nearly 70% of those over 50 experience some form of joint discomfort. (CDC)
But the good news is that joint pain after 50 is inevitable, and you can do a lot to feel better and prevent further damage. Below is a rundown of why your joints ache after 50 and, more importantly, what you can do about it immediately.
Who This Guide is For
- Active adults 50+ who want to maintain mobility.
- Retirees seek to stay independent and energetic.
- The initial planners are keen to avoid knee problems from getting worse than they already are.
Whether experiencing occasional twinges or daily stiffness, this guide gives you the necessary knowledge (and action plan).
Why Your Joints Ache After 50 (+ Surprising Factors You Didn’t Know)
1. Natural Aging Changes
Every joint within our bodies undergoes natural aging processes, leading to joint pain.
- Cartilage thinning represents a major factor in the development of symptoms because the flexible tissue that cushions the bone ends gradually breaks down. The absence of cartilage between bones creates close bodily contact that leads to joint pain as well as stiffness.
- Synovial fluid, which functions as the joint lubricant, experiences a decline during this process. This less fluid leads to increased friction.
Imagine it: Similar to the worn-out shoe soles that lose their shock-absorbing feature with time, deteriorating joints become less flexible and this makes daily activities painful and harder to perform.
2. Osteoarthritis (OA): The Silent Culprit
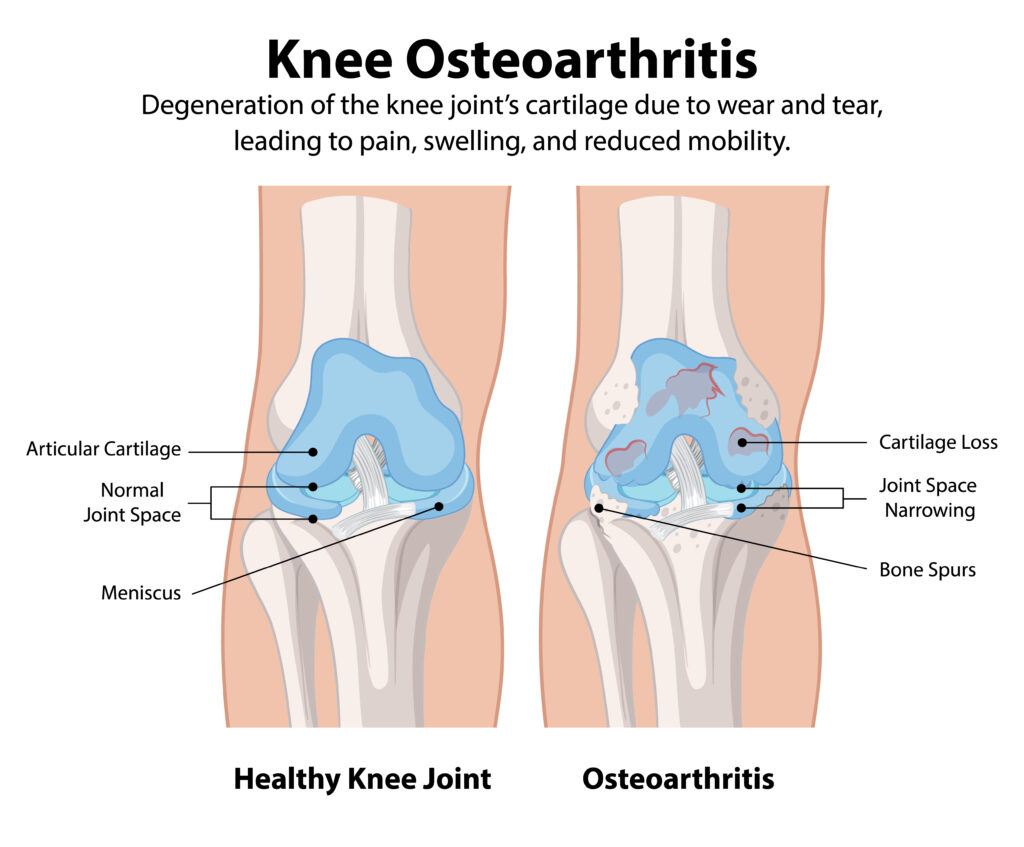
Osteoarthritis is the most common form of arthritis and a major source of joint pain onset after age 50. Scientists currently view OA as a disease comprising cartilage degeneration and chronic inflammation, although previously, people believed it came from “wear and tear.” The Arthritis Foundation indicates that OA exists in more than 32.5 million Americans, while the population with this condition increases substantially as people get older.
Typical symptoms include morning stiffness lasting over 30 minutes, joint swelling, and a grinding or crunching feeling when moving (crepitus). OA gradually worsens over time but can considerably affect movement and quality of life unless treated.
The main indicators of this condition are prolonged morning pain lasting half an hour or longer and joint swelling alongside audible noises during movements (crepitus). The degenerative nature of OA causes permanent health issues which severely restrict normal movement unless patients receive proper medical care.
3. Inflammation and “Inflammaging”
The term “inflammaging” refers to the slow buildup of persistent minor inflammation, which intensifies throughout older age and directly affects joint discomfort. As people age, their immune system reduces effectiveness in maintaining a fight against disease processes, which generates continuous low-level joint-damaging inflammation that occurs without detectable causes.
Inflammaging increases when a person experiences diet-related or stress-induced inflammation together with sleep problems and minimal physical activity. The concentration of C-reactive protein (CRP) in blood tests tends to increase after a person turns 50 years old through the process of underlying inflammation.
If left unmanaged, inflammation doesn’t just lead to joint pain — it also raises the risk of heart disease, diabetes, and cognitive impairment. Inflammation needs to be controlled for healthy aging and pain-free joints.
4. Muscle Loss and Joint Instability
Muscle strength is important for maintaining stable and protected joints. Unfortunately, after age 50, we automatically lose approximately 1–2% of muscle mass per year — a state referred to as sarcopenia. Weaker muscles mean joints have to bear more of the body’s weight and pressure without sufficient support.
This imbalance raises the risk for joint instability, misalignment, and injury such as sprain or tendonitis. Weak quadriceps, for instance, place enormous stress on knee joints, worsening symptoms of arthritis.
Regular strength training, even minimal resistance exercises, can reverse muscle loss, improve joint support, and significantly diminish pain and stiffness with age.
5. Resurfacing of old injuries
Old wounds don’t heal overnight — they tend to remain hidden beneath the surface and return with a vengeance after 50. Scarring tissue, ligament looseness, cartilage wear and tear, or changed biomechanics due to earlier sports injuries or accidents can present long-term weaknesses in joints.
As we get older and natural joint support decreases, these weak spots from years ago become more apparent, causing pain, swelling, and limited motion. For example, a long-forgotten ankle sprain in your twenties may suddenly cause your knees or hips to ache decades later.
Knowing your injury history and seeing a physical therapist can help you strengthen weak areas and avoid further joint problems.

What You Can Do About Joint Pain After 50 (Action Plan)
1. Keep Moving — Smartly
When it comes to aging joints, the old saying “motion is lotion” couldn’t be more true. Gentle, regular movement boosts the production of synovial fluid, lubricating and nourishing your joints naturally. Low-impact exercises such as swimming, tai chi, cycling, and light strength training are great options that safeguard your joints while keeping you active.
Pro Tip: Always warm up before working out and cool down afterwards to avoid unnecessary stress or injury. Skipping these steps will leave joints stiff and aching. Moving smartly keeps you mobile and pain-free for many years to come.
2. Opt for Joint-Friendly Nutrition
Diet is critical in controlling joint pain after the age of 50. An anti-inflammatory diet calms joints, restores tissues, and reduces systemic inflammation. Include foods such as salmon (rich in omega-3s), berries (with high antioxidant properties), leafy greens (teeming with calcium and vitamin K), and turmeric (whose active component, curcumin, battles inflammation).
Meanwhile, keep inflammatory culprits like processed foods, too much sugar, and trans fats at bay, which can make joint pain worse.
A natural, colorful diet of whole foods works like a healing balm for joints growing older, both providing immediate comfort and long-term protection.
3. Maintain a Healthy Weight
Joint health after the age of 50 is all the more important because weight control matters. Each additional pound gained roughly four pounds of extra pressure on your hips and knees. That’s stress that boosts cartilage erosion and intensifies pain.
The good news? Shedding as little as 5–10% of your body weight can make a big difference in reducing joint pain and increasing mobility. Small, gradual changes in your lifestyle, such as eating smaller meals, selecting whole foods, and remaining active, can make a huge impact.
Consider it this way: less weight = less stress = healthier joints. Maintaining healthy joints begins with maintaining a healthy body weight.
4. Strengthen Muscles Around Your Joints
Developing strong muscles gives your joints a “shield” that absorbs shock and avoids misalignment. After age 50, strength training becomes even more essential to offset the loss of muscle mass (sarcopenia). Targeted exercises such as:
- Wall sits for knee strength,
- Resistance band exercises for the shoulders, and
- Hip bridges for the hips and lower back should be emphasized.
Pro Tip: Emphasize eccentric exercises*(the slow lowering phase of movements). They strengthen tendons and ligaments more effectively and offer better joint protection.
Regular strength training isn’t about becoming a bodybuilder — it’s about fortifying your frame to stay pain-free and independent.
5. Consider Joint Supplements (With Caution)
Supplements such as glucosamine, chondroitin, collagen peptides, and curcumin have become popular for relieving joint pain. Research indicates that they have the ability to reduce the pain and enhance mobility, particularly in the initial stages of osteoarthritis. However, they’re not miracle cures and don’t work for everyone.
Always consult your healthcare professional before taking supplements, particularly if you are on medicati ons or have health conditions. Certain supplements can interact with blood thinners or other medications.
Consider supplements as support tools, not as alternatives to exercise, healthy food, or doctor visits. A balanced, prudent approach provides the best long-term outcomes.
6. Protect Joints in Daily Life
Small daily habits can either protect or punish your joints. Be a joint defender by:
- sitting on ergonomic chairs that help maintain posture,
- shock-absorbing shoes that absorb each step, and strategies that reduce impact.
- Stay away from repetitive, jarring actions such as jumping on hard floors or stressing your joints with heavy lifting without good form.
Small changes — such as lifting with your legs rather than your back, or taking breaks when sitting for long periods — can make a big difference in reducing wear and tear.
Consider it this way: guarding your joints every day keeps pain from becoming a permanent houseguest.
7. Seek Early Medical Intervention
If pain in joints begins to interfere with hobbies, work, or everyday activities, don’t grit and bear it. Early medical assessment can get ahead of issues before they worsen.
Choices such as physical therapy can instruct you in specific exercises to help build joints stronger. Treatments such as hyaluronic acid injections (to lubricate) or platelet-rich plasma (PRP) therapy (to trigger healing) become more effective at earlier levels of joint wear and tear.
Surgery, such as joint replacement, is always a last option, but early detection could prevent them from occurring in the first place.
Early action is your greatest friend when it comes to maintaining joint health.
Bonus: New Therapies for Joint Health
Hopes are high that revolutionary breakthroughs will revolutionize joint care. “Stem cell therapy” has potential in “regenerating arthritis-damaged cartilage” by reusing the body’s own repair cells. Initial reports indicate it could stall the advance of arthritis.
In the meantime, “gene therapy” remains in experimental phases, seeking to attack arthritis at the molecular level, potentially stopping the disease in its tracks before it can wreak havoc.
Though these treatments are not yet mainstream, they hold genuine promise for the millions of people suffering from chronic joint pain.
Stay up to date — the best days for joint health may be ahead (and better than you imagine)!
FAQs About Joint Pain After 50
Q: Is joint pain a natural part of aging?
A: No! While certain changes are natural, lifestyle plays a huge role in minimizing or postponing joint pain.
Q: What is the best vitamin for joint health?
A: Vitamin D, Vitamin C, and Vitamin K are important to joint and bone health.
Q: Do glucosamine supplements work?
A: Some research indicates modest benefits, but findings are variable. They work better for mild to moderate symptoms.
Q: When do I need to see my doctor?
A: If pain lasts longer than a few weeks, restricts movement, or results in swelling or redness, seek assessment.
Conclusion:
You’re Not Powerless — You’re Empowered!
Joint aches after 50 aren’t a life sentence. With the proper combination of exercise, diet, and preventive care, you can guard your joints, soothe pain, and have an active, healthy life well into your golden years.
Ready to get started? Begin with only 10 minutes of gentle stretching today and see the difference!
Also Read: “Top 10 Anti-Inflammatory Foods For Joint Pains”
Ergonomics for Remote Workers: Boost Comfort, Health, and Productivity from Home
Key Takeaways: Taking Care of Joint Pain After 50
- Aging naturally affects joint health by thinning the cartilage, swelling the joints, and losing muscle mass — but it’s not unavoidable that pain has to overtake your life.
- Gentle, consistent movement such as swimming, tai chi, and cycling keeps the joints lubricated and flexible.
- Anti-inflammatory foods like salmon, berries, greens, and turmeric can reduce joint pain.
- Maintaining a healthy weight takes unnecessary stress off your knees, hips, and back.
- Strength training stabilizes joints and prevents injuries as muscles lose strength with age.
- Supplements like glucosamine and collagen may aid joint comfort, but talk to your doctor before starting them.
- Simple daily adjustments, from better shoes to ergonomic chairs, can protect your joints in the long run.
- Early medical treatment with physical therapy or injections can slow or even reverse joint damage.
- New therapies like stem cell and gene therapy hold promising options for the future of joint well-being.
👉 Remember: Your body will grow older, but chronic joint pain doesn’t have to be. With smart and early actions, you can stay active, strong, and pain-free well into your 50s, 60s, and beyond!