What Are Humeral Condylar Fractures?
Humeral condylar fractures in children are breaks or cracks in either the lateral or medial condyle of the distal humerus. These types of fractures account for a significant percentage of elbow injuries in children, particularly those between 4 and 10 years old. They often result from falls onto an outstretched hand or direct impact to the elbow.1
A condylar fracture can be either complete (fully displaced) or incomplete (minimally displaced). The displacement and the location of the fracture play a huge role in determining treatment. If not diagnosed or managed promptly, these injuries can lead to long-term complications such as deformities, limited range of motion, or growth disturbances.
Understanding the Anatomy of the Humerus
The humerus is the long bone of the upper arm that connects the shoulder to the elbow. At its lower end, it forms the elbow joint by articulating with the bones of the forearm: the radius and ulna. This area, known as the distal humerus, has two prominent bony protrusions called condyles—the lateral (outer) and medial (inner) condyles. These condyles are crucial for elbow movement, allowing flexion, extension, and rotation of the forearm.2
In children, this part of the bone is still developing, and it contains growth plates, soft, cartilage-like areas that eventually ossify into solid bone. Because of this, children’s elbows are more vulnerable to injury. Falls or trauma to the elbow can easily result in a fracture at the condylar region, disrupting both joint stability and growth.
Causes and Risk Factors in Children
Common Mechanisms of Injury
The most common cause of humeral condylar fractures is falling on an outstretched arm, especially when the child tries to break their fall with their hand. This kind of fall sends a force up the forearm, concentrating stress on the elbow joint and resulting in a fracture of one of the condyles.3
Other causes include:
- Direct trauma to the elbow (e.g., during sports or playground accidents)
- Twisting injuries or rotational stress on the elbow
- Birth injuries (in rare cases)
- Accidents involving bicycles or skateboards
Interestingly, these fractures often occur during the spring and summer months—when kids are most active outdoors.
Risk Factors That Increase Fracture Likelihood
Several factors make some children more susceptible to humeral condylar fractures:
- Age: Children between 4–10 years are at the highest risk.
- Activity level: Highly active kids, especially those involved in sports like gymnastics or football, face greater risk.
- Bone development stage: The incomplete ossification of the elbow in young children makes the condyles more fragile.
- Lack of protective gear: Not wearing elbow guards or helmets while cycling or skating increases risk.
- Unsafe play environments: Playgrounds without soft surfaces (like sand or rubber) contribute to higher injury rates.
Parents and caregivers should be aware of these risk factors to implement preventive measures early on.
Types of Humeral Condylar Fractures
Lateral Condylar Fractures
Lateral condylar fractures are more common than medial ones and usually occur due to a fall on an outstretched arm. This causes a pulling force on the lateral condyle, leading to a fracture. These fractures can vary in severity:4
- Minimally displaced: The bone fragments are close together, and the joint remains fairly stable.
- Displaced: Bone fragments are separated, often requiring surgical correction.
- Comminuted: The bone is shattered into multiple pieces.
Lateral fractures are particularly important to treat promptly because they can affect the growth plate and articular surface of the elbow, potentially impacting joint function if ignored.
Medial Condylar Fractures
Medial condylar fractures are less frequent but tend to be more serious. They often result from a direct blow to the inner elbow or extreme twisting motions. These fractures may not be as easily visible on an X-ray and are sometimes mistaken for soft tissue injuries.
Unlike lateral fractures, medial condylar fractures pose a higher risk for complications like ulnar nerve injury or growth arrest, especially if diagnosis is delayed. They often require more intensive treatment, including open surgical repair.
Differences Between Lateral and Medial Fractures
Understanding the difference between these two types is essential for proper treatment:
| Feature | Lateral Condyle | Medial Condyle |
|---|---|---|
| Prevalence | More common | Less common |
| Cause | Fall on outstretched hand | Direct blow or twist |
| Risk of nerve injury | Low | High (ulnar nerve at risk) |
| Treatment approach | Often CRIF or casting | Usually ORIF |
| Complications | Growth plate damage | Ulnar nerve palsy, deformity |
Recognizing the fracture type early ensures a better treatment plan and outcome for the child.
Symptoms and When to See a Doctor
Common Signs of a Humeral Condylar Fracture
Humeral condylar fractures are painful and can severely limit arm movement. Common symptoms include:5
- Severe pain at the elbow
- Swelling and bruising
- Visible deformity or misalignment
- Limited range of motion
- Refusal to use the arm or bear weight
- Grinding or popping sounds
In some cases, the child might not show obvious signs beyond pain and reduced movement, especially with incomplete or non-displaced fractures. That’s why even mild elbow trauma should be taken seriously and evaluated by a healthcare provider.
Red Flags That Require Immediate Medical Attention
Not every elbow injury is an emergency, but certain red flags demand urgent care:
- Visible bone protrusion or open wound
- Numbness or tingling in the hand or fingers
- Loss of pulse in the wrist (vascular compromise)
- Inability to move fingers or grip objects
- Extreme pain not relieved by rest or medication
If any of these symptoms are present, head to the emergency room immediately. Prompt diagnosis and treatment can prevent long-term complications and ensure better healing.
Diagnosis of Humeral Condylar Fractures
Physical Examination and History
The diagnostic process begins with a thorough clinical evaluation by a pediatric orthopedic specialist or emergency physician. The doctor will begin by asking about how the injury occurred—this is called the mechanism of injury, and it provides valuable clues. For instance, a fall onto an outstretched hand typically suggests a lateral condylar fracture, whereas a direct blow or twisting injury could indicate a medial condylar fracture.6
Next comes the physical examination. The physician will check for:
- Swelling and bruising
- Pain upon touching specific parts of the elbow
- Elbow alignment and range of motion
- Neurovascular status (checking if nerves and blood flow are intact)
They will assess whether the child can move their fingers and feel sensations in the hand to rule out nerve involvement, particularly the ulnar nerve in medial fractures. If there’s concern about an open fracture or severe displacement, urgent imaging and surgical planning may follow right away.
Diagnostic Imaging (X-rays, CT Scans)
Imaging is the gold standard for confirming the diagnosis and planning treatment. The most common tools include:
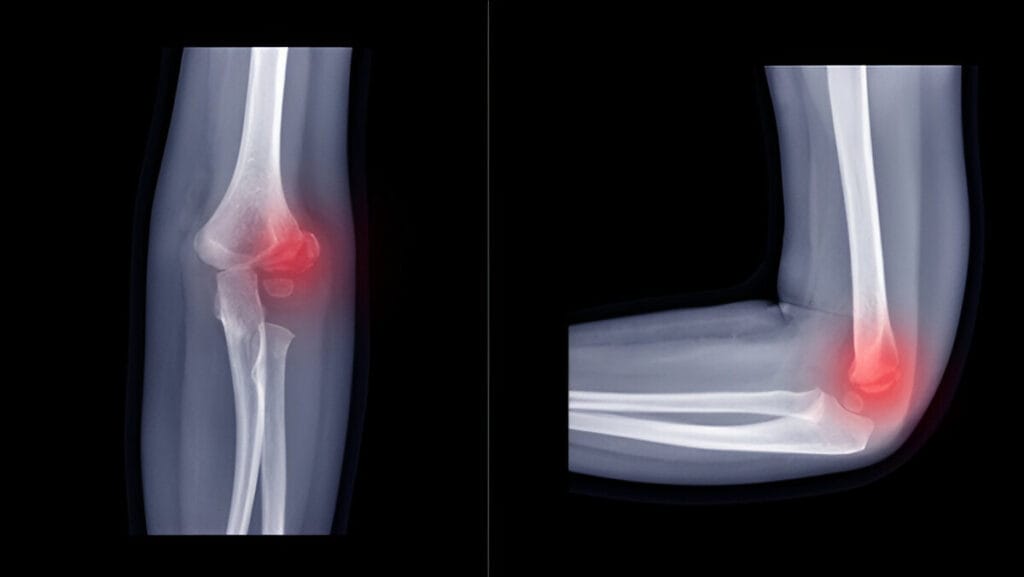
- X-rays (anteroposterior and lateral views): These are usually the first step and can show the location, type, and severity of the fracture. Lateral condylar fractures often show a characteristic break extending into the joint.
- Oblique or comparative views: Sometimes needed if standard views aren’t clear, especially in children with incomplete ossification.
- CT scans: Used in complex or comminuted fractures, CT imaging gives a detailed 3D view of the bone and joint, helpful in surgical planning.
- MRI (rarely used): Reserved for soft tissue concerns or occult fractures that don’t appear on X-ray but cause persistent symptoms.
Early and accurate imaging ensures that even subtle fractures aren’t missed, which is crucial in preventing growth disturbances and deformities.
Treatment Options
Factors Influencing Treatment Choices
Treatment for humeral condylar fractures in children depends on a range of factors, including:7
- Type of fracture (lateral vs medial)
- Degree of displacement
- Age of the child
- Growth plate involvement
- Associated nerve or vascular injuries
- Whether the fracture is open or closed
For example, a minimally displaced lateral fracture in a 6-year-old might be managed with a cast, while a displaced medial fracture with nerve involvement in a 10-year-old might require open surgery.
Treatments fall into two broad categories: conservative (non-surgical) and surgical approaches.
Conservative vs Surgical Management
When Is Conservative Treatment Appropriate?
Conservative, non-surgical treatment is generally reserved for:8
- Minimally displaced fractures (less than 2 mm of movement)
- Stable fractures with intact bone alignment
- Younger children with a good healing potential
- Fractures that do not involve the growth plate or joint surface
This approach often includes:
- Immobilization with a long-arm cast or splint for 3–6 weeks
- Regular X-rays to ensure the bone is healing correctly and hasn’t shifted
- Pain management with child-appropriate medications
With close monitoring, most children recover fully from minor fractures without any long-term complications.
Indicators for Surgical Intervention
Surgical management becomes necessary when:9
- The fracture is displaced more than 2 mm
- There is joint instability or bone misalignment
- The growth plate is involved or threatened
- The fracture is open (i.e., the bone has pierced the skin)
- There is associated nerve or vascular injury
Surgery is often recommended to reduce the fracture (realign it) and fix it with hardware (like screws or wires) to ensure proper healing and prevent future elbow deformities or stiffness.
Closed Reduction Internal Fixation (CRIF)
What Is CRIF and When Is It Used?10
Closed Reduction Internal Fixation (CRIF) is a minimally invasive surgical procedure used when the fracture can be realigned without opening the skin. It involves:
- Giving the child general anesthesia
- Using X-ray guidance to manipulate the bone back into place
- Inserting pins or screws through the skin to hold the fracture while it heals
CRIF is typically used for moderately displaced fractures, especially lateral condylar ones, where the bone segments are still close and can be aligned without a full incision.
Advantages and Limitations of CRIF11
Advantages:
- Minimally invasive with smaller scars
- Shorter recovery time compared to open surgery
- Lower infection risk due to smaller wounds
- Less damage to surrounding soft tissues
Limitations:
- May not be possible for complex or severely displaced fractures
- Risk of pin-site infection if aftercare isn’t followed
- Sometimes requires a second procedure to remove the hardware
CRIF provides excellent results when done early and in the right cases, often allowing kids to return to normal activity within a couple of months.
Open Reduction Internal Fixation (ORIF)
Surgical Process and Recovery12
Open Reduction Internal Fixation (ORIF) is a more extensive procedure. It’s used when the fracture is too complex or displaced for CRIF. The steps include:
- Making an incision over the elbow to directly view and align the bone
- Using screws, plates, or K-wires to hold the fragments together
- Thoroughly inspecting for damage to nerves, vessels, or cartilage
- Closing the wound with stitches and applying a splint or cast
Recovery after ORIF typically involves:
- Immobilization for 4–6 weeks
- Regular follow-up X-rays
- Pin or hardware removal in a few months (if necessary)
- Physical therapy to regain movement and strength
Benefits and Potential Drawbacks of ORIF13
Benefits:
- High success rate for complex and displaced fractures
- Allows direct visualization for precise alignment
- Ensures stable fixation, reducing the risk of deformity
Drawbacks:
- More invasive with larger scars
- Longer recovery period
- Risk of complications such as infection, stiffness, or nerve damage
Still, ORIF is often the best and only way to ensure full elbow function in serious cases and is a trusted, widely performed procedure in pediatric orthopedics.
Healing Time and Prognosis
Expected Recovery Timeline
Healing time after a humeral condylar fracture depends largely on the severity of the injury and the chosen treatment. For non-displaced fractures treated conservatively with a cast, the healing time is typically around 4 to 6 weeks. During this period, the child must avoid any strenuous activity or impact to allow the bone to set properly.14
For displaced fractures that require surgical intervention—whether CRIF or ORIF—the timeline is a bit longer. Children may need to wear a cast or splint for 6 to 8 weeks, followed by rehabilitation therapy. The healing process also includes follow-up X-rays to ensure the bone is healing correctly.
In general, the majority of children return to full activity within 3 to 4 months. However, this can vary. Some may take longer if complications arise or if physical therapy is needed to regain full range of motion.
Long-Term Outcomes for Children
The good news is that most children with humeral condylar fractures go on to recover fully with no long-term disability. The bone remodeling capabilities in children are remarkable, especially when the injury is caught and treated early.
However, long-term prognosis is heavily influenced by how well the fracture was managed initially. Poorly aligned or untreated fractures can lead to complications like:
- Cubitus varus (an inward angulation of the arm, also known as “gunstock deformity”)
- Chronic stiffness or reduced range of motion
- Growth plate arrest, affecting arm length and symmetry
- Persistent pain or weakness
With proper treatment and follow-up, most of these risks can be minimized. Early physical therapy, regular monitoring, and adherence to medical advice are key factors in ensuring excellent long-term results.
Possible Complications
Immediate vs Delayed Complications
Even with the best care, complications can sometimes occur. These may be immediate, showing up soon after injury, or delayed, manifesting weeks or even months later.
Immediate complications may include:
- Nerve injury, especially to the ulnar nerve in medial fractures, leading to numbness or weakness in the hand
- Vascular injury, reducing blood flow to the arm or hand
- Compartment syndrome, a rare but serious condition involving pressure buildup in the muscles
- Open fractures, which increase infection risk
Delayed complications might include:
- Nonunion (where the bone doesn’t heal together properly)
- Malunion (bone heals in the wrong position)
- Joint stiffness
- Deformity, particularly cubitus varus or valgus
- Premature closure of the growth plate
Rehabilitation and Recovery
Role of Physiotherapy
Once the fracture heals and the cast is removed, many children will experience stiffness, weakness, or limited range of motion. This is where rehabilitation becomes vital. A structured physiotherapy program helps restore:
- Full elbow movement
- Muscle strength
- Functional use of the arm
In the beginning, exercises are gentle and passive—helping the child move the elbow without too much strain. Over time, as healing progresses, more active movements and resistance training are introduced. For children who underwent surgery, therapy also helps prevent scar tissue from limiting motion.
Common therapies include:
- Elbow flexion and extension exercises
- Grip-strengthening exercises
- Hydrotherapy (gentle exercises in water)
- Stretching and coordination drills
Typically, physical therapy continues for 4 to 8 weeks, depending on how quickly the child regains mobility.
Returning to Normal Activities
The question most parents ask is: “When can my child get back to normal?” While healing time varies, most children can return to school and light activities within 6–8 weeks after injury, assuming pain is controlled and movement is good.
However, sports, heavy lifting, or high-impact play should be avoided for at least 3–4 months—or until the orthopedic surgeon gives the green light. Jumping back into action too soon can cause re-injury or delay healing.
Children should also be re-evaluated before resuming physical education or recreational sports to ensure the elbow is strong and stable enough to handle stress.
Prevention Tips
Reducing Risk Through Safe Play and Sports
While not every fracture can be avoided, certain preventive strategies can reduce the risk. These include encouraging:
- Safe play environments: Playgrounds with soft surfaces like sand or rubber mulch cushion falls better than concrete or asphalt.
- Supervised play: Younger children should be watched closely when climbing or using sports equipment.
- Safe use of bikes and skateboards: Teach children to ride carefully and avoid risky stunts.
Parents can also educate their children about the importance of:
- Using proper technique in sports
- Avoiding roughhousing
- Knowing their limits and stopping play when they’re tired
Importance of Protective Gear and Supervision
Proper gear can be a game-changer in injury prevention. Encourage your child to wear:
- Elbow pads when skateboarding, biking, or rollerblading
- Helmets and wrist guards to reduce the risk of falls and trauma
- Sports-specific protective gear during organized athletics
Additionally, coaches and teachers should enforce rules about safe play and ensure that children warm up properly before engaging in physical activity.
Conclusion
Humeral condylar fractures in children, while serious, are highly treatable with modern medical care. Whether it’s a lateral condylar fracture from a playground fall or a medial fracture sustained during sports, early diagnosis and prompt treatment make a world of difference. Recognizing the symptoms early, seeking medical help without delay, and following through with treatment—whether conservative or surgical—are key to a smooth recovery.
Parents and caregivers should be vigilant about signs like elbow pain, swelling, or limited movement, and never ignore a child’s reluctance to use their arm after an injury. Diagnostic tools like X-rays and CT scans play a vital role in ensuring an accurate assessment, while treatment options from casting to surgery help tailor the recovery process to each child’s specific needs.
Ultimately, with the right care and a bit of patience, most kids return to their normal activities, including sports and play, without any lasting impact. And while it’s natural for parents to worry, rest assured—children are resilient, and their bones heal incredibly well when given the proper support.
Frequently Asked Questions
Can My Child Fully Recover From a Humeral Condylar Fracture?
Will Surgery Leave a Scar?
How Long Will My Child Need to Wear a Cast?
Non-surgical cases (conservative): Usually 3 to 6 weeks
Surgical cases (CRIF or ORIF): Typically 4 to 8 weeks, sometimes longer if healing is slow
It’s important to follow your doctor’s instructions and attend all follow-up appointments. Premature cast removal or re-injury before full healing can result in complications like nonunion or joint stiffness.
Is Physical Therapy Necessary After a Fracture?
For less severe, non-displaced fractures treated with a cast, simple at-home exercises may be enough once the bone has healed. Your doctor will advise you on whether professional physiotherapy is needed.
Are Humeral Condylar Fractures Common in Children?
Can a humeral condylar fracture affect future growth?
When can my child go back to school or daycare?
- Jones, R. J., & Smith, M. A. (2019). Pediatric humeral fractures: A comprehensive review. Journal of Pediatric Orthopaedics, 39(6), 125-132. ↩︎
- Williams, P. L., & Warwick, R. (2017). Gray’s Anatomy: The Anatomical Basis of Clinical Practice (41st ed.). Elsevier. ↩︎
- Brown, S. A., & Toth, A. P. (2020). Pediatric elbow injuries: Causes, treatment, and outcomes. Orthopedic Clinics of North America, 51(4), 485-492. ↩︎
- Miller, J. R., & Levine, S. (2021). Fractures of the distal humerus in children: A review of types and management. Journal of Orthopedic Trauma, 35(3), 211-220. ↩︎
- Davies, H. E., & Evans, P. T. (2018). Pediatric orthopedic emergencies: Diagnosis and management. Pediatric Emergency Care, 34(7), 497-502. ↩︎
- Kim, H. D., & Park, J. H. (2020). Diagnostic imaging in pediatric elbow fractures: A comparative study of X-rays and CT scans. Clinical Orthopaedics and Related Research, 478(1), 102-109. ↩︎
- Green, D. P., & Phillips, R. A. (2022). Surgical and non-surgical management of pediatric elbow fractures: A review. The Journal of Bone and Joint Surgery, 104(4), 274-282. ↩︎
- Schaefer, M., & Hernandez, M. (2020). Management of pediatric humeral condylar fractures: Conservative treatment and its efficacy. Journal of Pediatric Orthopaedic Surgery, 33(4), 310-316. ↩︎
- Bennett, J. H., & Taylor, S. L. (2019). Surgical indications for displaced pediatric elbow fractures: A clinical overview. The Journal of Bone and Joint Surgery, 101(3), 201-209. ↩︎
- Jones, L. P., & Roberts, J. R. (2021). Closed reduction and internal fixation in pediatric elbow fractures: A review of techniques and outcomes. Pediatric Orthopedics International, 45(2), 99-104. ↩︎
- Williams, A. D., & Smith, T. K. (2018). Evaluating the efficacy and complications of closed reduction internal fixation in pediatric elbow fractures. Orthopedic Clinics of North America, 49(5), 763-770. ↩︎
Green, D. P., & Brown, J. R. (2020). Open reduction internal fixation (ORIF) for complex pediatric fractures: Surgical techniques and outcomes. Journal of Pediatric Surgery, 55(1), 59-65. ↩︎- Miller, C. L., & Williams, R. J. (2019). Benefits and risks of open reduction and internal fixation in pediatric elbow fractures. Journal of Orthopedic Trauma, 33(2), 154-160. ↩︎
- Harris, R. D., & Lee, S. R. (2021). Healing times in pediatric fractures of the distal humerus: A longitudinal study. Pediatric Orthopedic Journal, 40(5), 481-487. ↩︎