Glenohumeral Degenerative Joint Disease (GDJD) is a form of osteoarthritis that affects the ball-and-socket joint of the shoulder, where the head of the humerus (upper arm bone) meets the glenoid cavity of the scapula (shoulder blade). Like other types of arthritis, it involves the breakdown of cartilage, which cushions the bones in the joint. As the cartilage wears down, bone rubs against bone, leading to pain, inflammation, and decreased range of motion.
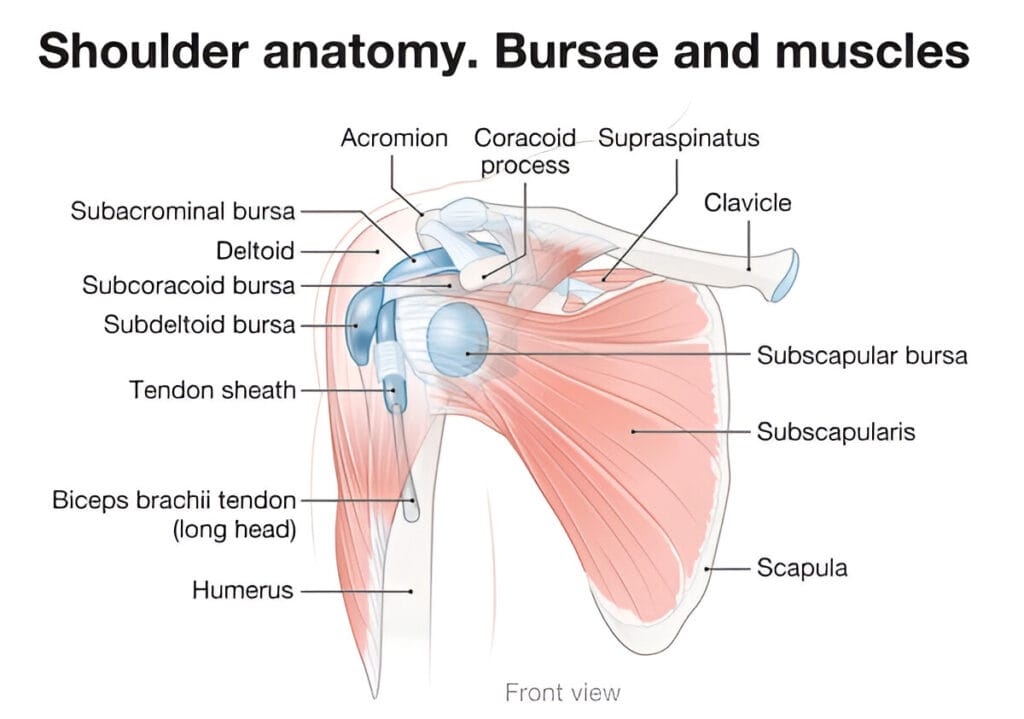
Glenohumeral Joint Anatomy
The glenohumeral joint, the main shoulder joint, is a ball-and-socket structure that enables extensive arm movement. The humeral head (ball) fits into the glenoid cavity (socket) of the scapula. While this design provides exceptional flexibility, it lacks deep structural stability, relying heavily on muscles, ligaments, and cartilage for support.
The joint is enclosed in a synovial capsule, which produces fluid to lubricate and cushion movement. However, this dependence on soft tissues and the joint’s shallow structure make it prone to wear and tear, particularly from overuse, poor posture, or injury.
Degenerative Joint Disease (DJD) also known as osteoarthritis, occurs when the cartilage covering the glenoid and humeral head erodes, leading to bone-on-bone contact. This causes pain, swelling, stiffness, and often the development of bone spurs (osteophytes).
DJD progresses slowly: symptoms begin with mild discomfort and worsen over time, potentially causing grinding sounds (crepitus) and significant loss of shoulder mobility. While not systemic like rheumatoid arthritis, DJD can severely impact daily activities. Early diagnosis and management are vital to maintaining joint function and quality of life.
What Is Glenohumeral Degenerative Joint Disease (GDJD)?
Glenohumeral Degenerative Joint Disease, as the name suggests, specifically targets the shoulder joint. It’s a form of localized osteoarthritis that gradually wears down the protective cartilage in the glenohumeral joint, leading to pain, stiffness, and decreased shoulder function.
This condition is the result of years of microtrauma, overuse, or degeneration. As the cartilage degrades, the joint loses its smooth, gliding motion. Inflammation sets in, and the once-fluid motion of the shoulder becomes painful and restricted.
Common Terms and Synonyms (Shoulder Osteoarthritis)
GDJD is often referred to in simpler terms, like:
- Shoulder Osteoarthritis
- Shoulder Arthritis
- Degenerative Arthritis of the Shoulder
Doctors might also classify it under primary or secondary osteoarthritis, depending on its cause. Primary GDJD develops with age and wear. Secondary forms are linked to specific causes like trauma, surgery, or congenital conditions.
Causes and Risk Factors of GDJD
Primary vs. Secondary Causes
Primary GDJD typically develops as part of the natural aging process. The more you use your shoulder over the decades, the more stress is placed on the joint structures. Eventually, the cartilage wears thin, leading to classic osteoarthritic changes.
Secondary GDJD, on the other hand, is triggered by specific events or conditions, such as:
- Previous shoulder injuries (like fractures or dislocations)
- Surgical interventions
- Rotator cuff tears
- Inflammatory conditions (like rheumatoid arthritis)
These incidents accelerate the breakdown of joint cartilage, sometimes leading to DJD at a much younger age.
Risk Factors Like Age, Injury, Genetics, and Lifestyle
Several risk factors increase your chances of developing GDJD:
- Age: The older you are, the higher the risk.
- Joint injuries: Even minor injuries can set the stage for degeneration.
- Repetitive use: Sports or occupations requiring frequent overhead motions (like painters, athletes, mechanics).
- Genetics: Family history of osteoarthritis increases susceptibility.
- Obesity: Though the shoulder isn’t weight-bearing, extra weight can still lead to inflammation and strain.
- Smoking: Reduces blood supply to joints, impairing healing and cartilage health.
Knowing these risks can help you take early action, even before symptoms appear.
Symptoms of Glenohumeral DJD
Pain and Stiffness
Pain and stiffness are hallmark symptoms of Glenohumeral Degenerative Joint Disease. Initially, pain occurs after activity but may become constant, even at rest, as the condition worsens. It often presents as a deep, dull ache in the shoulder, which can radiate to the upper arm or elbow, and may turn sharp with certain movements.
Stiffness is most noticeable after inactivity—like upon waking—making daily tasks such as dressing or reaching difficult. Joint inflammation contributes to discomfort, and in advanced stages, night pain can disrupt sleep. Together, pain and stiffness progressively impair shoulder mobility and daily function.
Decreased Range of Motion and Clicking Sounds
As cartilage deteriorates, bone-on-bone friction limits shoulder mobility, making actions like lifting or rotating the arm painful and difficult. A common symptom is crepitus—clicking, popping, or grinding sounds caused by loose cartilage or bone fragments and bone spurs within the joint.
Though these signs may seem minor early on, they indicate ongoing degeneration and should not be ignored, as delayed treatment can worsen the condition and complicate recovery.
Diagnosis of Glenohumeral DJD
Clinical Examination
Diagnosis begins with a thorough clinical examination conducted by a healthcare provider, often an orthopedic specialist. During this exam, the doctor will ask about your medical history, including any prior shoulder injuries, surgeries, or chronic health conditions. They’ll also want to know about your pain—when it started, what makes it worse, and how it’s affecting your daily activities.
Physical tests will be performed to assess:
- Range of motion (how far you can move your arm in various directions)
- Muscle strength (especially the rotator cuff muscles)
- Joint tenderness and swelling
- Clicking or grinding during movement
These tests help the physician identify whether the issue is likely DJD or another condition like rotator cuff injury, bursitis, or frozen shoulder.
Imaging Techniques (X-ray, MRI, CT)
While a physical exam provides initial clues, imaging studies are essential to confirm the diagnosis and assess the severity of the degeneration. The most commonly used imaging tools include:
- X-rays: The first-line imaging test for DJD. X-rays reveal narrowing of the joint space (due to cartilage loss), formation of osteophytes (bone spurs), subchondral sclerosis (hardening of the bone under the cartilage), and cyst formation.
- MRI (Magnetic Resonance Imaging): Useful for evaluating soft tissues, including the rotator cuff, labrum, and joint capsule. An MRI can show cartilage thinning or tears and fluid buildup in the joint.
- CT Scans: Occasionally used to get a more detailed view of the bone structures when surgery is being considered.
These imaging tests help your doctor determine the extent of the joint damage, which is essential for creating an effective treatment plan. The earlier the diagnosis, the more options you have to manage or even reverse the effects of the disease.
Stages of Glenohumeral Degenerative Joint Disease
Early Stage Characteristics
In the early stages, symptoms are often mild and easy to dismiss. You might experience:
- Occasional shoulder discomfort, especially after activity
- Mild stiffness that improves with gentle movement
- Slightly reduced range of motion
- Minimal to no visible joint changes on X-rays
Despite the subtlety of these symptoms, damage is already beginning inside the joint. The cartilage starts thinning, and the synovial fluid may become less effective at lubricating the joint. This is the best time for intervention, as early treatment can delay or even halt further degeneration.
People in the early stage often benefit greatly from physical therapy, lifestyle changes, and over-the-counter pain relief. But since the symptoms are mild, many people don’t seek treatment until the disease has progressed.
Advanced Stage Symptoms and Joint Damage
In the advanced stages, the damage becomes more pronounced and debilitating. Key symptoms include:
- Chronic, persistent pain, even at rest
- Severe stiffness, especially in the morning or after inactivity
- Dramatic reduction in shoulder mobility
- Visible swelling and possible deformity of the joint
- Increased frequency and intensity of clicking or grinding sounds
X-rays at this stage will show significant joint space narrowing, large osteophytes, and possibly deformity of the bone ends. The humeral head may become flattened, and the socket may develop abnormal contours due to constant wear.
At this point, conservative treatments often offer limited relief. Surgical intervention—such as shoulder replacement—may be necessary to restore mobility and relieve pain. The goal becomes not just managing pain, but also preserving the ability to perform essential daily tasks.
Treatment Options for GDJD
Conservative Treatments (Rest, Physical Therapy)
Initial treatment often focuses on conservative methods that aim to relieve symptoms without surgery. These include:
- Rest and activity modification: Avoiding activities that worsen symptoms can reduce inflammation and pain.
- Ice and heat therapy: Ice helps reduce swelling, while heat relaxes tight muscles.
- Physical therapy: A custom exercise program can strengthen the shoulder muscles, improve flexibility, and increase joint stability.
- Chiropractic care: Moves stiff joints within their natural range to reduce pain.
- Supportive devices: Braces, slings, or shoulder supports can offload stress from the joint.
These treatments are especially effective in the early stages of GDJD and may delay the need for surgical options.
Medications and Pain Management
For those with moderate symptoms, medications can provide significant relief. These include:
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Like ibuprofen or naproxen to reduce inflammation and pain.
- Corticosteroid injections: Directly into the shoulder joint to decrease inflammation and provide temporary relief.
- Hyaluronic acid injections: Less common but used to lubricate the joint and improve movement.
- Topical analgesics and muscle relaxants: Can also be used for short-term pain relief.
Pain management strategies may also include alternative therapies like acupuncture, TENS units, or chiropractic adjustments.
Surgical Options (Arthroscopy, Shoulder Replacement)
When non-surgical methods are no longer effective, surgery becomes the best option. Surgical treatments for GDJD include:
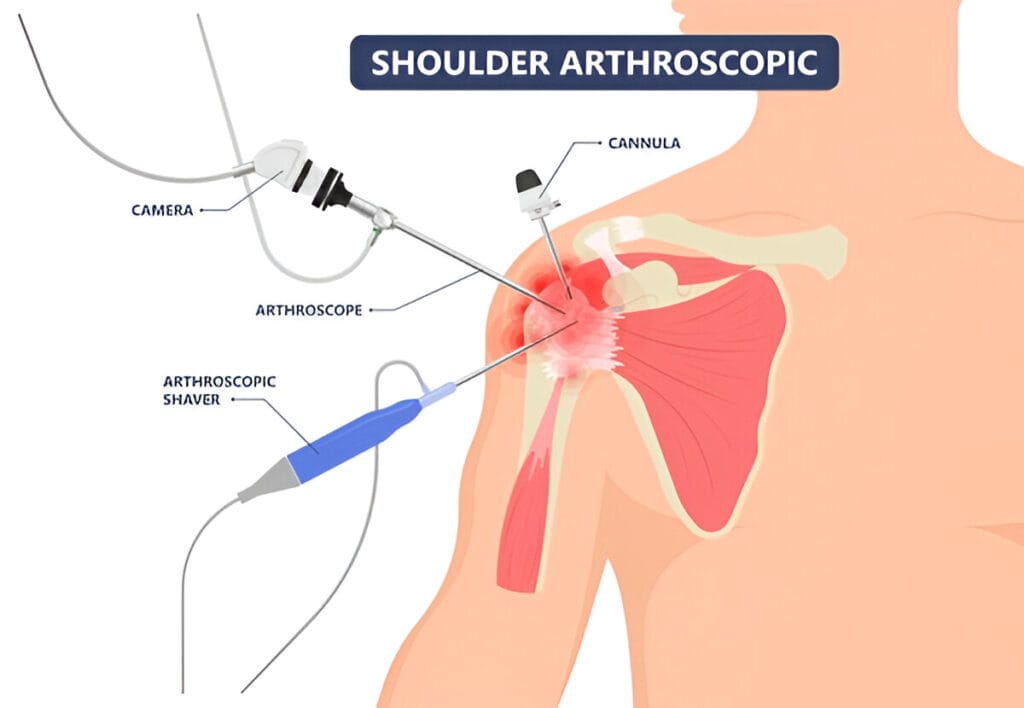
- Shoulder arthroscopy: A minimally invasive procedure used to remove bone spurs, loose cartilage, or clean out the joint.
- Hemiarthroplasty: Replacement of only the humeral head (ball), often used when the glenoid is still relatively healthy.
- Total shoulder replacement (Arthroplasty): Both the humeral head and glenoid cavity are replaced with prosthetic components. This is the gold standard for advanced GDJD.
Post-surgical rehabilitation is essential to regain strength and range of motion, and most patients see a dramatic improvement in pain and function.
Physical Therapy and Rehabilitation
Strengthening and Flexibility Exercises
Physical therapy is a cornerstone of managing Glenohumeral Degenerative Joint Disease, particularly in its early and moderate stages. A well-structured physical therapy program focuses on restoring mobility, strengthening surrounding muscles, and improving joint function without putting undue stress on the shoulder.
Therapists typically begin with gentle range-of-motion (ROM) exercises, which help combat stiffness and keep the joint from becoming “frozen.” As pain allows, they’ll introduce strength-building routines that focus on the rotator cuff and scapular stabilizers. Strengthening these muscles is essential because they support and stabilize the shoulder joint, relieving stress from the deteriorating cartilage.
Common physical therapy movements may include:
- Pendulum swings
- Wall crawls
- Isometric exercises
- External and internal rotations using resistance bands
Flexibility is another priority. Tight shoulder muscles can restrict movement and cause postural problems, making the joint work harder. Stretching the pectorals, deltoids, and upper back can significantly improve function and reduce pain.
Consistency is key. Doing your exercises daily, even if just for 15–20 minutes, can lead to noticeable improvements in mobility, strength, and pain reduction.
Role of Physiotherapists in Managing GDJD
Physiotherapists play a critical role in long-term joint health. They don’t just prescribe exercises; they analyze your movement patterns, identify weaknesses or compensations, and adjust your program as needed.
Beyond exercises, they also provide:
- Manual therapy to reduce stiffness and improve blood flow
- Ultrasound therapy for tissue healing
- Electrical stimulation (TENS) for pain relief
They’ll also educate you on body mechanics and posture to prevent further stress on the shoulder. A good physiotherapist tailors each program to your unique needs, adjusting intensity based on your condition’s severity and progression.
With regular sessions and dedicated home practice, many people with GDJD can avoid surgery for years—or even indefinitely.
Lifestyle Changes and Home Remedies
Weight Management and Diet
While your shoulder isn’t a weight-bearing joint like your knees or hips, excess body weight can still worsen GDJD by contributing to overall systemic inflammation. Fat cells release chemicals called cytokines that increase joint inflammation and accelerate cartilage breakdown. Some natural pain killers have a role, but not immediate relief.
A healthy, anti-inflammatory diet can help manage these symptoms and protect your joints. Focus on foods that are:
- Rich in omega-3s, like salmon, flaxseeds, and walnuts
- High in antioxidants, such as berries, leafy greens, and tomatoes
- Low in processed sugars and refined carbs, which can trigger inflammation
Supplements like glucosamine and chondroitin, though debated in effectiveness, may also offer relief for some individuals.
Long-Term Outlook and Prognosis
Can It Be Cured or Just Managed?
Unfortunately, Glenohumeral Degenerative Joint Disease is not reversible—once cartilage is lost, it doesn’t grow back. That said, the condition is highly manageable. With the right mix of treatments—physical therapy, lifestyle adjustments, and in some cases, surgery—most people can live active, functional lives.
The key is early detection and intervention. If you catch it early and make consistent efforts, you can slow the progression significantly. Conservative treatments work best when the disease is in its initial phases. As it advances, surgical options may become more necessary to restore joint function and alleviate pain.
Quality of Life Considerations
The impact of GDJD on quality of life can vary widely. Some people experience only mild discomfort, while others face debilitating pain that affects sleep, work, and personal activities.
Emotional health is also a factor. Chronic pain and reduced mobility can lead to frustration, depression, and anxiety. That’s why a comprehensive treatment plan should address not only the physical but also the psychological aspects of the disease.
Joining support groups, engaging in mental health counseling, and talking openly with healthcare providers about the emotional burden can improve your overall outlook and coping abilities.
Glenohumeral DJD in Athletes and Active Individuals
Sports-Related Causes
Active individuals and athletes, particularly those involved in overhead sports (like baseball, tennis, or swimming), are at a heightened risk of developing GDJD. The constant repetition of overhead arm motions places excessive strain on the glenohumeral joint.
In younger athletes, repetitive microtrauma may go unnoticed until pain or stiffness sets in. Over time, labral tears, rotator cuff injuries, or impingement syndromes can develop, accelerating cartilage wear and leading to early-onset DJD.
It’s common in athletes to dismiss mild pain as “just soreness,” but ignoring these early signs can lead to long-term damage. Identifying the issue early is crucial to preventing irreversible deterioration.
Return-to-Activity Guidelines
Managing GDJD doesn’t mean the end of athletic life. With proper guidance, many athletes can continue training and competing at high levels. The key lies in modifying activity, focusing on form and technique, and strengthening supporting muscle groups.
Return-to-activity recommendations often include:
- Limiting high-impact, repetitive motions
- Incorporating cross-training to reduce shoulder strain
- Using supportive gear like compression sleeves or shoulder braces
- Working closely with a physical therapist or athletic trainer
In cases of severe GDJD, athletes may require surgical intervention followed by a carefully monitored rehabilitation program. Though performance may be affected, many athletes return to their sport with modified routines and continued physical therapy support.
Prevention Tips for Glenohumeral DJD
Early Intervention
Preventing GDJD starts with listening to your body. Don’t ignore early signs of pain or stiffness. Seek evaluation early if you experience shoulder discomfort that doesn’t resolve within a few weeks.
Early interventions can include:
- Posture correction
- Rotator cuff strengthening
- Avoiding repetitive strain
- Routine stretching and joint mobilization
Preventing shoulder joint degeneration is much easier than treating it once it’s advanced.
Joint Protection Techniques
Practicing joint preservation techniques can dramatically reduce your risk of developing GDJD. These include:
- Using proper form when lifting or reaching
- Balancing activities to avoid overuse of one arm
- Maintaining flexibility through regular stretching
- Taking frequent breaks during repetitive tasks
Also, building a strong upper body helps cushion and support your shoulder joint. Focus on balanced strength training, avoiding overloading the shoulder with unbalanced or explosive exercises.
Taking care of your joints isn’t just about avoiding pain today—it’s about ensuring mobility and independence in the years ahead.
Conclusion
Glenohumeral Degenerative Joint Disease is more than a clinical term—it’s a daily challenge that can affect anyone, from athletes to retirees. It can gradually limit your mobility and quality of life.
The good news? With early diagnosis, consistent treatment, and lifestyle adjustments, it’s manageable. By understanding your shoulder, spotting symptoms early, and staying proactive with care, you can preserve function and avoid major interventions.
You’re not alone—health professionals and support communities are here to help. With the right approach, you can maintain shoulder health and keep doing the things you love.