What is Fibrodysplasia Ossificans Progressiva (FOP)?
Fibrodysplasia Ossificans Progressiva (FOP) is one of the rarest and most disabling genetic conditions known to medicine. Affecting about 1 in 2 million people worldwide, FOP is caused by a mutation in the ACVR1 gene. This mutation causes the body’s repair system to malfunction, turning soft tissues like muscles, ligaments, and tendons into rigid, bony structures over time.
This mutation is typically spontaneous, meaning it isn’t inherited from a parent but occurs as a new genetic change in the affected individual. However, the mutation is highly consistent across cases, most commonly affecting the same spot on the gene. The disease typically begins in early childhood and progresses throughout a person’s life.
FOP is often misdiagnosed, particularly in its early stages. Misdiagnosis can lead to harmful interventions, such as biopsies or surgeries, which accelerate the disease. Understanding the genetic roots of FOP is critical to avoiding these risks and managing the condition effectively.
How It Affects Soft Tissues and Bones
FOP not only affects bones, but it also redefines the way the body forms them. Normally, bones form through a highly regulated process during development and healing. In FOP, the mutated ACVR1 gene hijacks this process, leading the body to form bone in places where it shouldn’t.
This condition leads to heterotopic ossification (HO), the formation of bone in muscles, tendons, and connective tissues. Over time, these new bone formations fuse joints and muscles, severely limiting mobility and causing significant pain. In the context of the toes, even the smallest injury, like stubbing a toe or an insect bite, can initiate a painful flare-up and trigger ossification.
The condition is progressive, meaning it gets worse with time. There is no known cure, and all current treatments are focused on symptom management and injury prevention.
Anatomy of the Toe and FOP Interference
Normal Toe Structure
To understand how FOP affects the toe, it’s important to first know the toe’s normal anatomy. Each toe (excluding the big toe) typically consists of three small bones called phalanges: proximal, middle, and distal. These bones are connected by two joints, which allow for a surprising range of movement. The big toe has two phalanges and one joint.
Surrounding these bones are tendons and ligaments that control movement and provide stability. Muscles in the foot and leg help manipulate the toes, while blood vessels and nerves ensure proper circulation and sensation. The toe is covered by skin and topped with a nail that serves both protective and sensory functions.
The toe’s anatomy is compact, making it extremely sensitive to injury or structural changes. Even minor alterations can significantly affect balance, walking, and overall mobility.
Also Read: Ultimate Guide to Arthritis of the Big Toe Treatment
How FOP Disrupts Toe Functionality
In FOP, the delicate balance of the toe’s anatomy is disrupted. Ossification can occur in the connective tissues around the joints, gradually replacing them with bone. This leads to joint stiffness and eventually fusion, where two bones become one, eliminating the joint.
In the toes, this can start with inflammation, swelling, and pain, especially after trauma. As bone forms where it shouldn’t, it begins to lock the joints in place, making even simple tasks like walking, running, or wearing shoes increasingly difficult.
The tendons that allow toe flexion and extension become rigid, severely limiting motion. Over time, the foot may become misshapen due to uneven bone growth, which can lead to added stress on other joints and bones in the body.
Symptoms of FOP in the Toe
Early Signs and Indicators
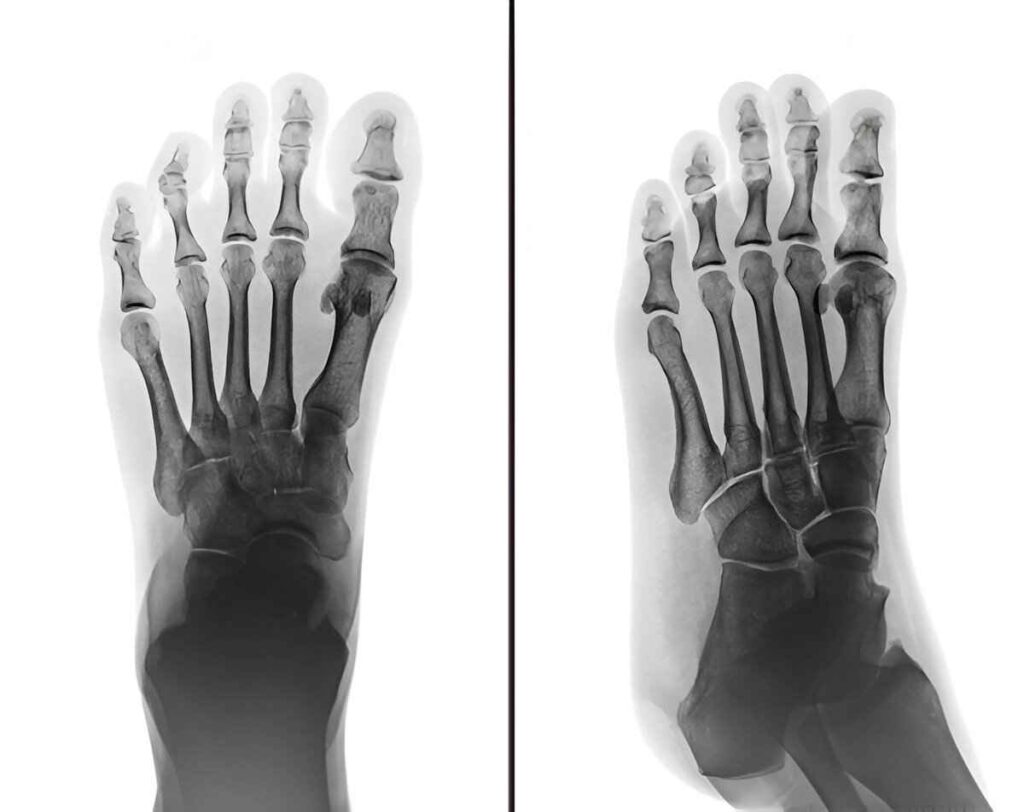
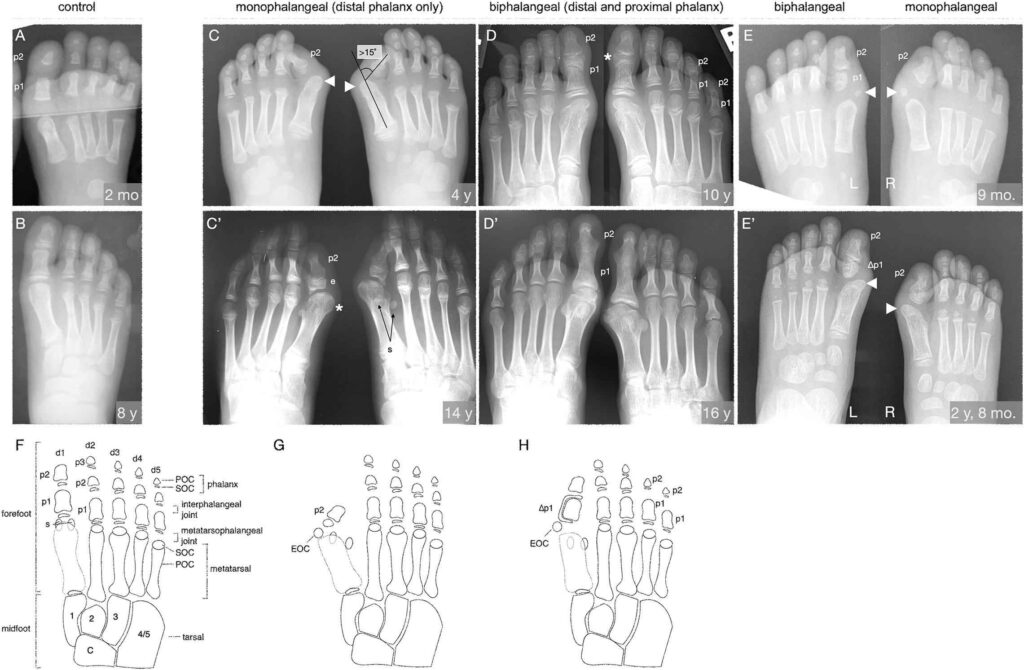
One of the most telling early signs of FOP is a congenital malformation of the big toe. Often, affected individuals are born with shortened, bent, or misshapen big toes that may point inward or have missing joints. These signs are sometimes mistaken for minor birth defects or orthopedic issues.
As the child grows, painful lumps or swellings may appear near the joints or under the skin of the toes. These lumps are often the start of a flare-up, during which inflammation sets the stage for ossification. The affected toe might become red, warm, and tender to the touch, resembling an infection or localized trauma.
Parents and caregivers often dismiss these early signs, especially if the child is otherwise healthy. But recognizing them is crucial for early diagnosis and preventing harmful interventions like surgery or biopsy, which can rapidly worsen the condition.
Progressive Symptoms Over Time
Without intervention, the symptoms worsen. Over months or years, the affected toe may begin to stiffen, swell permanently, and lose its natural shape. Walking becomes painful and difficult as the toe loses its flexibility. Footwear may become increasingly uncomfortable or impossible to wear.
Additional flare-ups can lead to cumulative damage, each new event forming more bone and further immobilizing the toe. In many cases, the toe becomes completely fixed in place, often at an awkward or non-functional angle.
Other symptoms like nerve pain, hypersensitivity, and pressure sores can emerge as the anatomy of the foot is further altered. Timely action can reduce unnecessary trauma and slow the progression of joint fusion.
Toe Joint Complications in FOP
Joint Stiffness and Mobility Loss
The hallmark of FOP is the gradual loss of joint mobility due to ossification. In the toe, this begins subtly. The joints become harder to move, and slight stiffness might be dismissed as a minor sprain or strain. Over time, this stiffness increases until the joints are completely locked.
This stiffness is caused by bone forming within the connective tissue and muscle that support the toe’s movement. Since there is no way for the body to remove this bone naturally, each flare-up becomes a step closer to complete immobility.
Loss of mobility in the toe affects balance and posture. The body compensates by shifting weight, which can cause further issues in the knees, hips, and spine. In extreme cases, the toe may become a solid mass of bone, completely fused and immobile.
Development of Bone Bridges
“Bone bridges” are connections of newly formed bone across the flexible joints. In the toes, these bridges often form between phalanges, locking the bones in place. These structures are not just cosmetic deformities; they’re functional roadblocks.
Once a bone bridge forms, it cannot be undone without surgery, which in the case of FOP, could trigger even more bone formation. As these bridges spread, they can extend into adjacent toes or even into the foot, creating a chain reaction of immobility.
Patients may also experience pressure ulcers or secondary infections due to unnatural pressure points formed by rigid, misaligned toes. Bone bridges are one of the most disabling aspects of FOP, making prevention and flare-up management critical.
Nail and Skin Changes with FOP in the Toe
Toenail Irregularities
The toenail reflects changes in health, circulation, and structural alignment of the toe. In FOP patients, toenail abnormalities can develop due to pressure from bone growth or improper blood flow caused by distorted anatomy.
Nails may thicken, become discolored, or grow at odd angles. Ingrown toenails are especially problematic, as they can lead to infections that trigger new flare-ups. Sometimes, the nail may lift away from the nail bed due to swelling or pressure from underneath, which is both painful and difficult to treat.
Routine care and monitoring of toenails are essential. Avoiding trauma, using soft, rounded nail tools, and consulting a podiatrist familiar with FOP are all critical for managing nail health.
Skin Sensitivity and Secondary Effects
As the toe becomes more rigid, the skin over and around it can suffer. Skin may become overly tight, dry, or cracked due to pressure from underneath. In some cases, circulation issues may lead to discoloration or ulcer formation.
FOP-affected toes often have heightened sensitivity, meaning that even light touch or mild rubbing from a sock or shoe can cause pain. These areas also heal more slowly, increasing the risk of infection and compounding the damage caused by flare-ups.
Preventative skin care is important. Use soft, moisture-wicking socks, avoid harsh soaps, and apply gentle moisturizers daily. Monitoring the skin for signs of irritation or infection can prevent small issues from becoming major complications.
Causes and Triggers of FOP Toe Flare-Ups
Genetic Mutation and How It Works
Fibrodysplasia Ossificans Progressiva (FOP) is rooted in a genetic mutation, specifically, the ACVR1 gene. This gene is responsible for regulating bone growth through the BMP (bone morphogenetic protein) pathway. In FOP patients, this gene becomes overactive, triggering soft tissue, like muscles, tendons, and ligaments, to convert into bone.
In the toe, this means that even a small injury or spontaneous flare-up can result in unwanted bone formation. The body’s natural repair system backfires, confusing healing with ossification (bone growth). This mutation is present from birth, even though symptoms might not become apparent until early childhood.
Physical Trauma and Infection as Catalysts
Something as a stubbed toe, minor surgery, or even an insect bite can set off a painful FOP flare-up. Physical trauma is the number one external cause. Infections can also contribute by increasing inflammation, which is a known precursor to heterotopic ossification (HO).
If you’re dealing with FOP in the toe, it’s crucial to avoid unnecessary trauma. Even standard procedures like vaccinations or blood draws in affected areas can trigger ossification. For toes, this becomes even more crucial, as they’re prone to injury from everyday walking or wearing tight shoes.
Pain Management in FOP-Affected Toes
The Nature of Pain in FOP
The pain in FOP is a deep, aching, often burning sensation caused by inflammation, nerve compression from new bone growth, and tissue tension. In the toe, this pain is magnified due to the limited space and the network of nerves and joints.
This pain can become chronic, impacting walking and weight-bearing activities. Even resting doesn’t always alleviate the discomfort, especially during active flare-ups. Understanding that this pain is both physical and neurological helps in managing it more effectively.
Medical and Natural Approaches to Relieve Pain
The focus is on managing symptoms. NSAIDs (non-steroidal anti-inflammatory drugs) like ibuprofen may help reduce inflammation and pain during a flare-up. Corticosteroids are sometimes prescribed in the very early stages of a flare to reduce inflammation quickly.
For natural pain relief, warm soaks, gentle massage with essential oils, or using padded footwear can help minimize discomfort. Some patients also turn to therapies like acupuncture or guided meditation to manage chronic pain. However, always consult a specialist before trying new treatments, especially physical therapies.
Infection Risks and How to Handle Toe Infections in FOP
In people with FOP, the skin and underlying tissues are more vulnerable due to inflammation and structural deformities. This can make them more prone to skin breakdown, ulcers, or fungal infections, especially around the toes and toenails. Any infection can act as a catalyst for a flare-up.
The challenge lies in treating infections without triggering more ossification. Even something as routine as cleaning a wound or applying pressure can spark bone growth.
Managing Toe Infections Safely and Effectively
Prevention is key. Keep the toes clean, dry, and protected. Avoid clipping nails too short or digging into the sides of the nail beds. If an infection does occur, it should be managed with the utmost caution.
Antibiotics might be necessary, but should be administered under medical supervision. Never attempt home surgeries like draining pus or removing ingrown toenails. Seek help from a healthcare provider experienced in dealing with FOP.
Podiatric care from a specialist who understands the condition is essential. Using antiseptic soaks, antibiotic creams, and proper wound dressing can make a world of difference without escalating the risk of ossification.
Surgical Intervention: Why Surgery is Risky for FOP Toes
Surgery is typically avoided in FOP patients unless necessary. Why? Because any invasive procedure, even a simple biopsy or mole removal, can cause massive flare-ups and irreversible bone growth.
This is particularly dangerous in the toes, where space is limited and functionality is delicate. Surgical removal of bone or correction of deformities often results in even more bone growth in the same or surrounding areas, worsening the problem.
Are There Any Safe Surgical Options?
Some research into gene therapies and soft-tissue preservation surgeries shows promise, but we’re not there yet. In the meantime, surgical intervention should only be considered in life-threatening scenarios or when the risk of not operating outweighs the damage it might cause.
In extreme cases where the toe becomes infected or necrotic (dead tissue), amputation might be considered, but only after exhausting all other options. Even then, ossification can spread into the residual limb.
The Link Between Neurofibromatosis and FOP
Though FOP and Neurofibromatosis (NF) are separate genetic disorders, they sometimes get confused due to overlapping symptoms like lumps under the skin and joint stiffness. However, they’re fundamentally different. NF causes tumors on nerve tissues, while FOP results in bone formation in soft tissues.
Patients diagnosed with one might be screened for the other, especially if unusual symptoms are present. Proper genetic testing is the only way to confirm a diagnosis.
Managing Both Conditions if Diagnosed Concurrently
If someone happens to have both FOP and NF (an extremely rare situation), management becomes more complex. It’s essential to have a multidisciplinary team including geneticists, neurologists, and orthopedic specialists to balance both conditions without triggering complications in either.
Long-Term Impact of FOP on Toe Mobility
Gradual Immobilization and Its Daily Effects
Over time, FOP can drastically reduce toe mobility. What begins as slight stiffness can evolve into complete fusion of joints. This results from the progressive ossification of ligaments and tendons around the toe, eventually turning them into bone. In practical terms, it means that the toe becomes fixed in one position, often awkwardly bent or protruding.
This rigidity affects more than just walking. It changes your gait, balance, and posture, potentially leading to further complications in the knees, hips, or spine. Tasks that once seemed simple, like wearing shoes, standing for long periods, or exercising, become physically challenging or impossible.
Orthotic and Assistive Devices for Improved Movement
Custom-made shoe inserts, toe separators, and padded footwear can help distribute pressure evenly and minimize pain during walking. These aids are especially useful during the early and middle stages of FOP progression.
As mobility decreases, assistive devices like walking sticks, crutches, or mobility scooters might become necessary. Occupational therapists can help tailor these tools to suit individual needs, ensuring safety without compromising independence.
Patients should also consider gentle, low-impact activities to maintain circulation and muscle tone, swimming or seated stretching routines are usually safe. Consulting a physiotherapist who understands FOP is essential to avoid flare-ups while staying as active as possible.
Injury Prevention Strategies for FOP-Affected Toes
Proactive Steps to Avoid Trauma
Since trauma is one of the leading causes of FOP flare-ups, preventing injuries is paramount. The toes, being constantly exposed during walking or physical activity, are particularly at risk. Here are some key precautions:
- Always wear protective, well-fitted shoes.
- Avoid barefoot walking—even indoors.
- Place soft padding around bedposts or furniture corners.
- Use non-slip mats in bathrooms and kitchens.
- Be cautious on stairs and rough terrain.
Even seemingly harmless actions, like stubbing a toe or dropping a small object, can trigger ossification. Taking daily precautions may seem excessive, but it’s a small price to pay to avoid lifelong complications.
Educating Family and Caregivers
Living with FOP isn’t a solo journey. Family members, caregivers, and close friends must understand the seriousness of the condition. Educating them about safe handling, appropriate footwear, emergency protocols, and infection control measures will foster a safer environment.
Make sure those around you know what to do and what not to do in case of an injury. They should avoid applying pressure, moving the limb unnecessarily, or attempting to “pop” or “fix” any misaligned joints or swelling. Creating a shared understanding reduces the risk of accidental trauma.
Toe Removal and Amputation Considerations in FOP
When Is Amputation Considered?
Amputation is considered only in rare, extreme cases, typically when the toe becomes severely infected or necrotic, and there’s no other way to protect the rest of the limb or body.
Because any surgical intervention can lead to explosive ossification, even successful toe removal may cause new bone growth at the surgical site or surrounding tissues. This can lead to more pain, deformity, and immobility than before the procedure.
Post-Amputation Care and Risks
Post-surgery, patients require intense monitoring to manage inflammation and prevent additional bone formation. Anti-inflammatory drugs, physical therapy, and strict wound care protocols are all part of the recovery process. Additionally, emotional and psychological counseling is crucial, as the trauma of amputation can deeply affect mental health.
Prosthetics are generally not recommended for FOP patients due to the risk of skin pressure and further trauma. Instead, special padding and modified footwear are used to help patients regain some mobility.
How to Care for Toenails in FOP Patients
For people with FOP, maintaining toenail health is both essential and challenging. The typical nail care routine, clipping, filing, and cleaning, needs a serious makeover to ensure it doesn’t trigger a flare-up. Even the slightest cut or pressure around the toenail area can lead to soft tissue trauma and potentially cause new bone to form.
Here’s how to care for your toenails safely:
- Use rounded-tip nail scissors or clippers, preferably ones designed for sensitive skin.
- Never cut the nails too short or dig into the corners.
- Soak the feet in warm water for 10–15 minutes before trimming to soften the nails and reduce pressure.
- Dry the toes thoroughly and apply an antiseptic ointment if there’s any redness or irritation.
If you notice any discoloration, thickening, or pain around the nail bed, consult a podiatrist immediately. Always avoid nail salons or untrained personnel for grooming. A podiatrist familiar with FOP is your best bet for safe and effective nail care.
Dealing with Ingrown or Infected Toenails
Ingrown toenails pose a serious risk in FOP patients. As the nail grows into the surrounding skin, it can create a minor wound, an open door for infections and inflammation. Unfortunately, the conventional treatment of surgically removing the ingrown portion is not advisable due to the risk of heterotopic ossification.
Instead, early intervention is key:
- Wear loose, breathable footwear.
- Apply antiseptic solutions at the first sign of swelling or redness.
- Soak in warm, soapy water with Epsom salts for 15 minutes a day.
- Use antibiotic ointment under medical guidance.
If the infection persists or worsens, immediate medical attention is necessary. A trained professional may use conservative techniques like lifting the nail edge with sterile cotton instead of surgical methods.
Importance of Early Diagnosis and Genetic Counseling
Identifying FOP in Infants and Children
As the child grows, painful swellings or lumps may appear near the neck, back, or limbs. These are often mistaken for tumors or aggressive forms of arthritis.
Misdiagnosis can lead to unnecessary biopsies or treatments, which in FOP patients can accelerate the progression of the disease. If FOP is suspected, genetic testing should be conducted immediately to confirm the presence of mutations in the ACVR1 gene.
Benefits of Genetic Counseling for Families
Once FOP is diagnosed, genetic counseling can help families understand the implications of the disease.
Genetic counselors provide invaluable insights into:
- The nature and cause of the mutation
- Future family planning options
- Risks of recurrence in siblings or offspring
- Access to FOP research trials and medical registries
Moreover, counseling offers emotional support, helping families navigate the psychological burden of a rare disease.
Future Treatments and Ongoing Research for FOP
Pharmaceutical Breakthroughs on the Horizon
One such approach is targeting the ACVR1 gene’s signaling pathway to prevent soft tissues from converting into bone. Drugs like palovarotene, a retinoic acid receptor gamma agonist, have shown potential in slowing bone growth during flare-ups.
Other studies are exploring antibodies and molecules that can block the BMP signaling pathways, thereby halting heterotopic ossification before it begins. While most of these treatments are still in experimental stages, the future looks more hopeful than ever before.
The Role of Personalized Medicine
Researchers are studying patient-specific factors, like disease progression patterns, to develop highly customized care plans.
In the future, AI-driven models may help predict flare-up risks, allowing for preemptive treatment. Until then, staying informed about new clinical trials and experimental therapies is essential. Many global foundations and research networks regularly update families and patients on progress in the field.
Conclusion:
Fibrodysplasia Ossificans Progressiva is more than a medical diagnosis—it’s a life-altering journey. When FOP affects the toe, it introduces unique challenges that impact mobility, hygiene, and overall quality of life. From managing pain and avoiding infections to choosing safe footwear and exploring future treatments, the road is far from easy.
But with early diagnosis, consistent care, and emotional support, people with FOP can still lead meaningful, fulfilling lives. Medical science is advancing, bringing us closer to better treatments—maybe even a cure. Until then, staying vigilant, informed, and connected with the FOP community is the best way forward.
You’re not defined by your condition. With courage, compassion, and community, you can keep moving forward—one step at a time.