When we talk about cervical myelopathy recovery time, the truth is, it depends. Quite a few things. But let’s narrow it down to the big three: how bad the compression is, what treatment path you’re on, and how your body was doing before all this started.
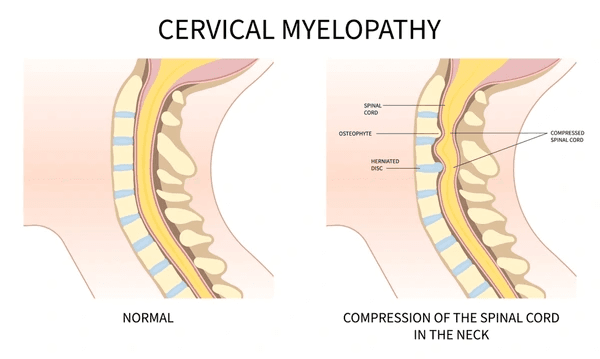
Severity of Spinal Cord Compression (Mild vs. Severe)
In mild cases of cervical myelopathy, where the spinal cord is just lightly pinched, you might bounce back in as little as three to six months, sometimes even without surgery.
But in severe cases, where there’s prolonged, intense pressure, it’s a different story. Nerves don’t regenerate like muscles. Once damaged, they take a long time to repair—if they can at all. And if the compression caused something called myelomalacia (spinal cord softening), recovery becomes more about managing symptoms than fully reversing them.
Patients with advanced myelopathy often have issues with fine motor skills, gait instability, and even bladder dysfunction. The more systems affected, the longer the road. You’ll need more time, more therapy, and, yes, more patience. Because as I always tell my patients, “Patience isn’t just a virtue here—it’s a prescription.”
Surgical vs. Non-Surgical Routes
If you’re wondering whether surgery fast-tracks your recovery, the answer is: not always—but it often stabilizes things before they get worse. The most common surgeries are ACDF (Anterior Cervical Discectomy and Fusion) and laminoplasty. These are designed to decompress the spinal cord and, in some cases, prevent permanent damage.
Surgical recovery can be grueling in the first few weeks—swelling, soreness, and fatigue are the norm. But for many, surgery halts the progression and offers a new baseline for healing. One 2023 Journal of Neurosurgery study found that 70% of ACDF patients regained full mobility within six months. 1
Non-surgical treatment, on the other hand, relies heavily on physical therapy, medication, posture correction, and pain management. It’s a slower grind, but it can work, especially for those with mild compression. Still, without the structural fix that surgery offers, recovery tends to be longer and more variable.
Age and Pre-Existing Health Conditions
Here’s a hard truth: recovery doesn’t play fair. A 35-year-old triathlete is going to heal faster than a 75-year-old with diabetes and arthritis. Age isn’t just a number when it comes to healing capacity; it’s a biological variable. As we age, our nerve conduction slows, our tissues regenerate more sluggishly, and inflammation takes longer to resolve.
But don’t get discouraged if you’re on the older side. I’ve had patients in their 60s recover beautifully—with the right plan, consistent therapy, and strong motivation. It’s just that the timeline may stretch a bit longer.
Comorbidities like diabetes, autoimmune conditions, or even smoking history can all complicate recovery. These factors slow tissue repair, increase inflammation, and sometimes increase the risk of complications post-surgery.
It means your body’s starting point sets it, your treatment path, and your daily choices. And we’ll get to those choices, like rehab and diet, in a bit.
Typical Recovery Timeline
Understanding the timeline of cervical myelopathy recovery depends on the route you’re taking—surgical or conservative. Here’s how recovery typically unfolds for the most common treatments.
ACDF Surgery: Weeks 1–6 vs. Months 3–6
Let’s talk about Anterior Cervical Discectomy and Fusion (ACDF)—the MVP of cervical myelopathy surgeries. This procedure removes the offending disc and fuses the vertebrae to keep things stable. But the moment you leave the OR, the real work begins. 2
Weeks 1–6: Expect stiffness, neck soreness, and a hard time swallowing during the first few days. You’ll likely be in a soft or hard cervical collar. You might start walking within the first 24 hours, but any lifting or heavy motion is strictly off-limits. Most patients return to light desk work around week 4 or 5, depending on pain and stamina.
Months 3–6: This is when fusion begins to solidify, and the swelling that’s been pressing on your spinal cord starts to recede. Nerve function may improve dramatically during this time, especially if the compression didn’t last too long before surgery.

You’ll likely be doing structured physical therapy, rebuilding strength, and fine-tuning your posture. One of my patients, a 52-year-old accountant, told me that it was during month 4 when he finally stopped dropping his coffee cup due to hand weakness. For many, this is the sweet spot where progress feels real.
Laminoplasty: Why Some Patients Recover Faster
Laminoplasty is often chosen for multilevel compression because it decompresses the spine without fusing it, meaning more motion is preserved. Surgeons hinge open the vertebrae like a door, relieving pressure while maintaining flexibility. That’s a big win if your lifestyle requires mobility (think athletes, musicians, or folks with physical jobs).
The recovery tends to be smoother than ACDF in some cases. Why? No fusion = no waiting for bone healing. That means less restriction in motion and sometimes less pain.
Patients usually return to light activities in 2–3 weeks and see functional gains within 2–3 months. But nerve healing still takes time, and the intensity of pre-op symptoms plays a big role. One marathon runner I treated regained jogging ability by month five, but only after relentless daily PT and posture correction.
Non-Surgical Rehab: When to Expect Improvements
If you’re skipping the knife, your timeline stretches a bit, but all hope is far from lost. Non-surgical treatment typically includes physical therapy, pain management, medication (like corticosteroids or nerve blockers), and ergonomic lifestyle changes.
Month 1: You’ll likely start to see modest relief—maybe a bit less tingling, slightly better coordination, or fewer spasms. But this depends on how disciplined you are with therapy.
Month 3: This is when real gains show up—reduced pain, better balance, and maybe even a return to part-time work.
Month 6 and beyond: Many patients plateau here, but that’s not necessarily bad. Your nerves may have reached their new normal. If symptoms are manageable, surgery might not be necessary. But if function hasn’t improved at all, your doctor may recommend reassessing the plan.
Red Flags vs. Progress Signs
Recovery can feel like two steps forward. Let’s break it down into the good, the bad, and the “call your doctor immediately.”
Positive Signs (e.g., Tingling Fading, Mobility Return)
Noticing tingling moving from your fingertips to your wrists? That’s good news. Nerve healing often travels in reverse order from how the symptoms appeared. So if you felt numb from the neck down and now just your hands tingle, that’s progress.
Other positive signs?
- Improved hand coordination (e.g., buttoning shirts without fumbles).
- Increased grip strength.
- Better gait and balance (e.g., no longer veering while walking).
- Reduced neck pain and stiffness.
One of the biggest wins is better proprioception, that’s your body’s ability to sense where it is in space. When this returns, you stop bumping into things and feel more “in control.” It’s subtle, but it’s a sign your spinal cord is recalibrating.
Red Flags (e.g., New Weakness, Incontinence)
Not everything that happens during recovery is normal. And waiting it out sometimes does more harm than good.
Red flags to watch for:
- Sudden weakness in your arms or legs (especially if it’s worse than before surgery).
- New or worsening numbness.
- Loss of bladder or bowel control.
- Difficulty breathing or swallowing beyond the first few days post-op.
- Persistent, worsening neck pain with fever (could indicate infection).
If any of these occur, don’t second-guess yourself—call your surgeon immediately. A delayed response can make all the difference in outcomes.
As a Johns Hopkins spine surgeon says, “Recovery plateaus aren’t failures, they’re part of the process. But new symptoms? That’s not a plateau. That’s a sign.”
How to Speed Up Recovery (Without Overdoing It)
Now that we’ve talked about what’s typical, when it comes to cervical myelopathy, more effort doesn’t always mean better outcomes.
PT Exercises to Avoid (e.g., Heavy Neck Rotations)
Here’s the deal: physical therapy is your best friend, but the wrong exercises. They’re your worst enemy. I’ve seen patients stall, or even regress, because they jumped into neck rotations or weighted chin tucks way too early.
Avoid these during early recovery:
- Deep neck flexion/rotation stretches
- Weighted resistance training on your neck
- Overhead lifting before 12 weeks (post-op)
- High-impact cardio (running, jumping)
Instead, opt for isometric neck holds, scapular retractions, and gentle range-of-motion drills. Your physical therapist should customize this based on your surgery type, symptom severity, and overall function.
Nutrition Tips for Nerve Healing
Inflammation is a major player in cervical myelopathy, and your diet can either tame it or feed it.
Top nutrients to prioritize:
- Vitamin B12 – crucial for nerve regeneration.
- Omega-3 fatty acids – found in salmon, chia seeds, flax.
- Magnesium – helps reduce nerve hypersensitivity.
- Antioxidants – berries, leafy greens, turmeric.
Try a nerve-healing smoothie: almond milk, banana, spinach, chia seeds, blueberries, and a scoop of collagen. Easy on the neck, easy on the gut, and packed with healing compounds.
Also, stay hydrated. Nerve tissues are sensitive to dehydration, which can worsen stiffness and cramping. Aim for at least 8–10 cups of water daily.
Expert Insights: What the Science Says
We’ve talked timelines, treatments, and tips—but what does the research say? Let’s take a closer look at the science behind cervical myelopathy recovery and what real data tells us.
Recent Study on Recovery Timelines (2023 Data)
A 2022–2023 retrospective study in Frontiers in Surgery comparing 116 patients found similar neurological improvements in both ACDF and laminoplasty at 24 months based on standardized outcomes like JOA, NDI, and VAS 3
- 70% of ACDF patients regained full mobility within 6 months
- A 2021 analysis of the Quality Outcomes Database (n ≈ 150) reported that laminoplasty patients returned to routine activities faster—47.2% by 3 months vs 21.2% for posterior cervical fusion.
- A systematic review noted higher neck pain rates in laminoplasty compared to other methods (5–20%) .
The study emphasized that earlier surgical intervention (within six months of symptom onset) was tied to better outcomes across all ages. So, the sooner the diagnosis and decompression, the more likely patients were to experience complete or near-complete recovery.
It also highlighted the plateau phase—most patients saw dramatic improvement in the first 6 months, followed by a slower progression from months 6 to 12. That’s crucial because many patients worry when they stop improving rapidly. But remember: plateau ≠ failure. It’s just the body’s way of stabilizing before the next gain.
Often Overlooked Recovery Factors
Here are two big ones:
Sleep Posture and Pillow Choice
I’ve seen patients delay their healing simply because they were unknowingly putting strain on their necks for 8 hours a night.
If you’re sleeping on a pillow that cranks your neck forward or doesn’t support the natural curve of your spine, you’re waking up already inflamed. Not the best way to start your day.
Ideal sleep setup:
- Use a cervical contour pillow (memory foam preferred).
- Sleep on your back with a small pillow under your knees to reduce spinal pressure.
- Avoid stomach sleeping at all costs—it rotates the neck awkwardly.
One study even showed that a proper pillow reduced morning stiffness by 30% in cervical myelopathy patients over 6 weeks. That’s no small win.
Stress and Mental Recovery
Anxiety, fear, and frustration aren’t just side effects—they actively interfere with healing.
How? Chronic stress increases cortisol, which fuels inflammation and slows nerve regeneration. Your body literally stays in fight-or-flight mode, which is the opposite of the calm environment your nerves need to repair.
What helps?
- Mindfulness meditation (even 10 minutes daily).
- Cognitive behavioral therapy (CBT) for recovery-related anxiety.
- Journaling progress to stay motivated.
Remember, recovery is physical and psychological. Treat both with the same care.
Life After Myelopathy: Returning to Normal
Patients often ask: “When can I get my life back?” The answer varies depending on how invasive your treatment was and how demanding your lifestyle is. Let’s explore two major milestones.
Can You Drive After Surgery?
Short answer: Yes, but not right away.
After ACDF or laminoplasty, most surgeons recommend waiting at least 2–4 weeks before driving. Why?
- Your neck mobility will be limited, especially if you’re wearing a brace.
- Pain meds (especially opioids) impair reaction time.
- Sudden movements or braking can stress healing tissues.
Your doctor will clear you to drive based on:
- Whether you’ve weaned off strong painkillers.
- Whether you can turn your head enough to check blind spots.
- Your ability to sit comfortably and react quickly.
Some patients feel ready by week 3. Others may take up to 6 weeks. Rule of thumb: If you hesitate, don’t do it. Better safe than re-injured.
When Can You Return to Work or Hobbies?
The answer depends entirely on what kind of work or hobby we’re talking about.
Office jobs: Most patients return to desk work within 4–6 weeks post-op. Just make sure your workspace is ergonomically sound.
Physical labor: You’ll need 3–6 months before lifting, climbing, or repetitive motion is safe again.
Hobbies: Gardening, golf, or painting? Usually okay by month 3. High-impact sports or heavy lifting? Likely 6–12 months or more.
Your surgeon or therapist should guide you through a graduated return-to-work program—because diving in too soon could undo months of progress.
Rehab Essentials: What You Should Know
Rehabilitation isn’t just a phase; it’s the heartbeat of your recovery. Whether you’re post-surgery or on a conservative path, rehab provides the structure your spine and nervous system need to recover, adapt, and thrive.
Physical Therapy Milestones by Month
Let’s break this down month by month, because progress isn’t always visible day to day, but it is trackable over time.
Month 1: Foundation Phase
- Focus: Pain control, inflammation reduction, gentle mobility.
- PT Goals: Learning safe neck positions, initiating core and scapular strengthening.
- You may feel sore, but trust the process; this phase is about setting up for success.
Month 2–3: Activation Phase
- Focus: Rebuilding basic motor control and posture correction.
- PT Goals: Improve neck range of motion, balance drills, light aerobic activity.
- You’ll likely notice better hand coordination and reduced numbness.
Month 4–6: Strength & Stability Phase
- Focus: Enhancing endurance, mobility, and function.
- PT Goals: Light resistance training, proprioceptive work, and cardio.
- This is when you feel more like yourself again.
Month 6–12: Return-to-Life Phase
- Focus: Safely resuming work, hobbies, and normal life.
- PT Goals: Sport-specific training (if needed), fine-tuning movements.
- For many, this is when the “new normal” becomes the “normal.”
Remember: PT isn’t about pushing harder—it’s about moving smarter. And always communicate with your therapist about setbacks or plateaus.
Equipment That Can Help
Sometimes a little gear can go a long way. Here’s a breakdown of rehab tools that can seriously boost your recovery:
| Equipment | Purpose | When to Use |
|---|---|---|
| Cervical Collar | Neck stabilization post-op | First 2–6 weeks |
| Resistance Bands | Progressive muscle strengthening | Months 2–6 |
| Foam Rollers | Posture correction, upper back release | Anytime (supervised) |
| TENS Unit | Pain and spasm control | As prescribed |
| Ergonomic Desk Setup | Prevent neck strain | Work-from-home setup |
These tools are not a substitute for therapy—but they’re powerful additions to your routine. Consult your PT before buying fancy gadgets.
5 Questions to Ask Your Surgeon About Recovery
Before you head into surgery—or even if you’re already post-op—it’s smart to go in prepared. Here are 5 essential questions you should ask your spine surgeon:
- What’s the expected recovery time for my specific condition?
- What activities should I avoid in the first 3 months?
- When can I start physical therapy, and what will it involve?
- What symptoms are red flags after surgery?
- Will I need imaging (MRI/X-ray) to track recovery progress?
Don’t feel shy, surgeons appreciate informed, engaged patients. And these questions aren’t just about peace of mind; they help you prepare your life around your recovery.
Surgical vs. Conservative Recovery Timeline
Let’s visualize what the typical timeline looks like for different treatment paths:
| Timeframe | ACDF Surgery | Laminoplasty | Non-Surgical Rehab |
|---|---|---|---|
| 0–2 weeks | Pain/swelling, collar use | Light activity | PT eval, rest |
| 1 month | Return to light tasks | Return to light tasks | Basic PT progress |
| 3 months | PT ramp-up, improved function | Moderate activity return | Moderate symptom relief |
| 6 months | Major mobility gains | High-functioning | Possible plateau |
| 12 months | Near-complete recovery | Long-term strength | Continued conservative care |
This chart is a guideline. Every patient progresses differently. But if you fall way outside these windows, that’s your cue to check in with your care team.
Conclusion
Cervical myelopathy recovery time is a journey, one that doesn’t follow a straight line. Whether you’re looking at 3 months or 12 months, the key lies in understanding your body, your treatment, and your habits. This isn’t just about healing a spine, it’s about restoring your life.
Some days you’ll feel on top of the world. Others, you’ll wonder if you’re moving backward. But with the right guidance, realistic goals, and steady rehab, you will make progress.
So, be kind to your body. Listen to your therapist. And remember: patience, not pressure, is what brings you back to life.
FAQs
How long to recover from cervical myelopathy after ACDF?
Most patients see major improvements within 3 to 6 months, with full recovery potentially taking up to 12 months. Initial pain resolves in the first 6 weeks, but nerve recovery takes longer.
What are signs you’re healing properly?
Positive signs include reduced tingling, improved coordination, better posture, and less neck pain. You should also see gradual increases in mobility and balance.
Can you recover without surgery?
Yes—if your condition is mild. Physical therapy, anti-inflammatories, posture correction, and lifestyle changes can improve symptoms. But moderate to severe cases often require surgery for meaningful recovery.
How does physical therapy help cervical myelopathy?
PT strengthens supportive muscles, improves posture, and helps restore movement patterns. It also relieves pressure on the spinal cord by teaching proper biomechanics.
What should I avoid during recovery?
Avoid heavy lifting, neck hyperextension, high-impact sports, and any unsupervised neck exercises. Also avoid poor sleep posture and skipping PT sessions.