Cervical disc herniation is a common spinal condition that may begin with a simple neck ache. Still, it can also cause debilitating symptoms affecting your arms, balance, and even bladder control. Often misdiagnosed, this condition can significantly reduce your quality of life, especially when the spinal cord is involved. However, with early diagnosis and proper treatment, most individuals can make a complete recovery.
This comprehensive guide aims to provide an in-depth understanding of cervical disc herniation—its anatomy, causes, symptoms, diagnostic procedures, and treatment strategies—empowering patients to seek timely and appropriate care.
What Is Cervical Disc Herniation?
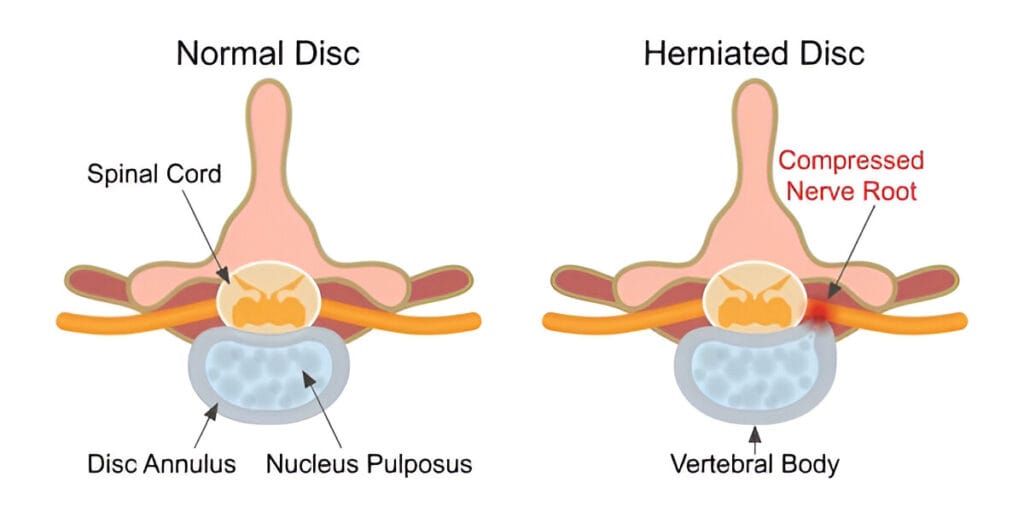
Cervical disc herniation occurs when the soft, gel-like core of a spinal disc (known as the nucleus pulposus) protrudes through a tear in its tough outer layer (the annulus fibrosus) in the neck region. This herniation may affect adjacent nerve roots or the spinal cord itself. Depending on the location and severity of this compression, individuals may experience a wide range of symptoms, from localized pain to serious neurological dysfunction.
The cervical spine comprises seven vertebrae (C1 to C7). Discs sit between these bones (except between C1 and C2) to allow flexibility and act as shock absorbers. When the disc herniates, the material that leaks out can press on sensitive neural structures, causing not only pain but also dysfunction in areas the affected nerves supply.
Anatomy of the Cervical Spine
To understand cervical disc herniation, it’s essential to appreciate the structure of the cervical spine.
1. Vertebrae and Discs
- The cervical spine consists of seven vertebrae (C1–C7).
- The C1 (Atlas) and C2 (Axis) vertebrae are structurally unique to allow rotational and nodding movements of the head.
- Intervertebral discs are located from C2-C3 down to C7-T1.
- Each disc consists of:
- Nucleus pulposus: a soft, gelatinous center.
- Annulus fibrosus: a tough, fibrous outer ring.
2. Facet and Uncovertebral Joints
- Facet joints, found at the back of the spine, permit controlled movement.
- Uncinate processes, small bony projections, help form uncovertebral joints, stabilizing the spine laterally.
3. Ligaments
Important stabilizing ligaments include:
- Anterior Longitudinal Ligament (ALL)
- Posterior Longitudinal Ligament (PLL)
- Ligamentum Flavum
4. Spinal Cord and Nerves
- The spinal cord passes through the spinal canal, giving rise to nerve roots that supply the shoulders, arms, and hands.
- Compression of these nerves or the spinal cord itself results in the symptoms associated with cervical disc herniation
Causes of Cervical Disc Herniation
Cervical disc herniation usually results from a combination of aging, mechanical stress, and traumatic events. While it may appear suddenly, the underlying degeneration usually develops gradually over years.
Common Causes Include:
- Degenerative Disc Disease (DDD)
- With age, intervertebral discs lose water content, elasticity, and structural integrity, making them more susceptible to herniation.
- Sedentary Lifestyle
- Physical inactivity reduces the diffusion of nutrients into the disc and hastens disc degeneration.
- Whiplash or Trauma
- High-velocity injuries, such as those from car accidents, can cause sudden tearing of disc fibers.
- Poor Posture and Repetitive Neck Movements
- Prolonged use of smartphones (termed “text neck”) or working at an improperly positioned computer screen contributes to cumulative stress on cervical discs.
- Heavy Lifting or Strain
- Improper lifting techniques or sudden strain (like violent coughing or sneezing) can rupture a compromised disc.
Symptoms of Cervical Disc Herniation
The symptoms of a cervical herniated disc vary based on the location and extent of nerve or spinal cord involvement.
1. Localized Neck Symptoms
- Persistent or intermittent neck pain
- Stiffness and reduced flexibility
- Pain that radiates to the upper back or shoulder blade area
2. Radiculopathy (Nerve Root Compression)
Occurs when the herniation impinges on a nerve root.
- Sharp, radiating pain in the arm
- Tingling, numbness, or burning sensation
- Muscle weakness in the affected limb
- Symptoms vary by nerve root:
- C5: Shoulder pain, deltoid weakness
- C6: Biceps weakness, thumb numbness
- C7: Triceps weakness, middle finger symptoms
3. Myelopathy (Spinal Cord Compression)
Myelopathy is a more severe form caused by compression of the spinal cord itself.
- Difficulty walking or maintaining balance
- Weakness or stiffness in legs
- Clumsiness or reduced fine motor control in hands
- Urinary urgency or bowel dysfunction (in advanced cases)
- Hyperreflexia or abnormal reflexes (e.g., positive Babinski or Hoffmann’s sign)
Diagnosis of Cervical Disc Herniation
A combination of clinical evaluation and imaging is necessary for accurate diagnosis.
1. Clinical Examination
- Assessment of neck movement and posture
- Neurological examination: reflexes, muscle strength, sensation, coordination
- Special signs: Romberg’s, Hoffmann’s, Spurling’s maneuver
2. Imaging Studies
- X-rays: Detect disc space narrowing and alignment problems
- MRI: Gold standard for visualizing disc herniation, nerve root, and spinal cord compression
- CT scans: Useful for identifying bone spurs or calcified discs
- EMG/NCV tests: Assess electrical activity and identify nerve damage when imaging and symptoms mismatch
Treatment Options for Cervical Disc Herniation
The choice of treatment for cervical disc herniation depends on several key factors:
- The severity and duration of symptoms
- The presence or absence of neurological deficits
- Whether the spinal cord (myelopathy) or nerve roots (radiculopathy) are involved
- The patient’s age, activity level, overall health, and response to initial conservative management
The treatment pathway usually begins conservatively and only escalates to surgical options when necessary.
1. Conservative Management
Conservative (non-surgical) treatment is usually the first line of defense, particularly when the herniation causes localized neck pain or mild nerve irritation without significant weakness or spinal cord involvement.
A. Medications
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs)
- Medications like ibuprofen, naproxen, or diclofenac reduce inflammation and provide pain relief.
- They are often used short-term due to risks like gastritis, ulcers, or kidney issues if taken chronically.
- Muscle Relaxants
- Drugs such as cyclobenzaprine or tizanidine help relieve muscle spasms often accompanying neck pain.
- These are typically prescribed for short durations to improve range of motion.
- Neuropathic Pain Agents
- Medications like pregabalin or gabapentin target nerve pain (tingling, burning, shooting pain).
- These are particularly useful for radicular symptoms, where nerve roots are irritated or compressed.
- Topical Agents and Patches
- Capsaicin creams or lidocaine patches may be used for localized symptom relief.
B. Physical Therapy
A structured therapy program aims to:
- Relieve pressure from nerve roots
- Improve neck mobility
- Strengthen cervical muscles
- Correct posture and alignment
Key modalities include:
- Cervical traction: Gentle pulling of the neck to relieve disc pressure
- IFT (Interferential Therapy): Low-frequency electrical stimulation to reduce pain and improve circulation
- Laser Therapy: Enhances tissue repair and reduces inflammation
- Ultrasound Therapy: Provides deep tissue heating and pain relief
- Manual Therapy & Mobilization: Hands-on techniques to improve joint movement
C. Lifestyle Modifications
Long-term improvement often hinges on changing harmful habits:
- Ergonomics:
- Use chairs with proper back and neck support
- Keep monitors at eye level to avoid forward head posture
- Use a standing desk or take frequent breaks
- Posture Correction:
- Regular reminders to avoid slouching
- Core and upper back strengthening exercises
- Sleep Positioning:
- Use a cervical pillow
- Avoid sleeping on the stomach, which strains the neck
- Activity Modification:
- Limit overhead lifting
- Avoid repetitive neck flexion (e.g., looking down at phones for long durations)
2. Radiculopathy Treatment
Radiculopathy occurs when a herniated disc compresses or irritates a cervical nerve root, leading to pain, numbness, or weakness in the arms.
A. Conservative First
In the absence of muscle weakness or progressive symptoms, conservative treatment is continued:
- NSAIDs and nerve pain medications
- Physical therapy and posture training
- Lifestyle changes to reduce neck stress
B. Corticosteroids
If symptoms persist or inflammation is significant:
- Oral steroids (e.g., prednisone taper)
- Intravenous steroids in acute cases
- Epidural steroid injections (interlaminar or transforaminal) under fluoroscopic guidance
- These can provide significant relief for weeks to months
- Repeated no more than 3 times a year to minimize side effects
C. Surgical Indications
Surgery becomes necessary when:
- Pain persists for 6–12 weeks despite conservative care
- Progressive weakness, loss of sensation, or loss of function appears
- MRI confirms significant nerve compression correlating with symptoms
3. Myelopathy Treatment
Cervical myelopathy is a serious condition resulting from spinal cord compression. Symptoms include imbalance, clumsy hands, and possible bowel/bladder dysfunction. Unlike radiculopathy, conservative treatment is often insufficient.
A. Why Surgery Is Necessary
- The spinal cord, once compressed, has limited regenerative ability
- Delay in treatment can result in permanent disability
- Early surgical intervention improves outcomes and halts progression
B. Non-surgical Measures
While they may temporarily ease symptoms, they do not prevent neurological deterioration. In very early myelopathy or in high-risk surgical patients, non-operative care may be considered cautiously and only under close monitoring.
Surgical Options for Cervical Disc Herniation
When conservative management fails, or neurological symptoms worsen, surgery is indicated. The choice of procedure depends on:
- The number of levels affected
- The direction of disc herniation
- Whether nerve roots or spinal cord are compressed
- The patient’s age, anatomy, and activity level
1. Anterior Cervical Discectomy and Fusion (ACDF)
Overview:
- Most commonly performed surgery
- Surgeon approaches from the front of the neck
- Removes the herniated disc and decompresses neural structures
- The disc space is filled with a bone graft or cage, and the vertebrae are fused
Advantages:
- Direct access to herniated material
- High success rate for pain relief
- Stabilizes spine, preventing further collapse
Risks:
- Limited neck motion at the fused level
- Risk of adjacent segment disease (increased stress at nearby discs)
2. Artificial Disc Replacement (ADR)
Overview:
- Alternative to fusion
- Disc is removed and replaced with a mobile artificial implant that preserves motion
Best Candidates:
- Younger, active patients
- Single-level disease
- No spinal instability or significant facet joint arthritis
Advantages:
- Maintains natural movement
- Reduces the risk of adjacent segment degeneration
Limitations:
- Not suitable for multilevel disease or deformity
- Limited long-term data compared to fusion
3. Endoscopic Discectomy
Overview:
- A minimally invasive technique
- A small tubular retractor and camera are inserted through a tiny incision
- Herniated disc material is removed with micro-instruments
Advantages:
- Less muscle damage
- Reduced hospital stay
- Faster recovery and less post-operative pain
Considerations:
- Technically demanding
- Suitable only for selective soft disc herniations, not severe stenosis or instability
4. Posterior Cervical Decompression (Laminectomy / Laminoplasty)
Posterior cervical decompression is used when:
- The spinal cord is compressed from behind
- Multiple levels are involved
- The spine is not kyphotic (curved backward)
A. Laminectomy
- The entire lamina (posterior arch of the vertebra) is removed
- Decompresses the spinal cord over multiple segments
- May be combined with fusion if instability is a concern
B. Laminoplasty
- Lamina is hinged open like a door to expand the spinal canal
- Maintains spinal motion without fusion
Advantages:
- Good for multilevel myelopathy
- Avoids anterior surgery and its risks
Drawbacks:
- May cause neck stiffness
- Higher risk of post-operative muscle atrophy
Why Early Diagnosis Matters
Time is a crucial factor in managing cervical disc herniation, particularly when spinal cord compression is present. Unlike peripheral nerves, the spinal cord has limited regenerative capacity. Prolonged compression may result in permanent disability.
Early recognition of symptoms such as imbalance, frequent tripping, difficulty with fine hand movements, or unexplained weakness should prompt immediate medical evaluation. Delaying surgery in cases of myelopathy may reduce the likelihood of full recovery, even after successful decompression.
Preventive Measures and Lifestyle Recommendations
While not all cases are preventable, the risk of cervical disc herniation can be reduced through:
- Maintaining a healthy weight to reduce spinal load
- Regular physical activity, especially core and neck strengthening
- Avoiding prolonged screen use without breaks
- Practicing proper lifting techniques
- Ensuring ergonomically optimized workspaces
Final Thoughts
Cervical disc herniation is not merely a neck problem; it’s a potentially disabling condition that can significantly alter your ability to work, perform daily activities, or live independently. While mild cases often respond to conservative treatments, symptoms like arm weakness, coordination loss, or balance difficulty may signify more serious spinal cord involvement and should be taken seriously.
The good news is that with early diagnosis and tailored treatment—whether conservative or surgical—most patients recover well and regain their function. If you’re experiencing persistent neck pain or any neurological symptoms, seek evaluation from a spine specialist to prevent further complications and safeguard your quality of life.