What Is Carpal Tunnel Syndrome?
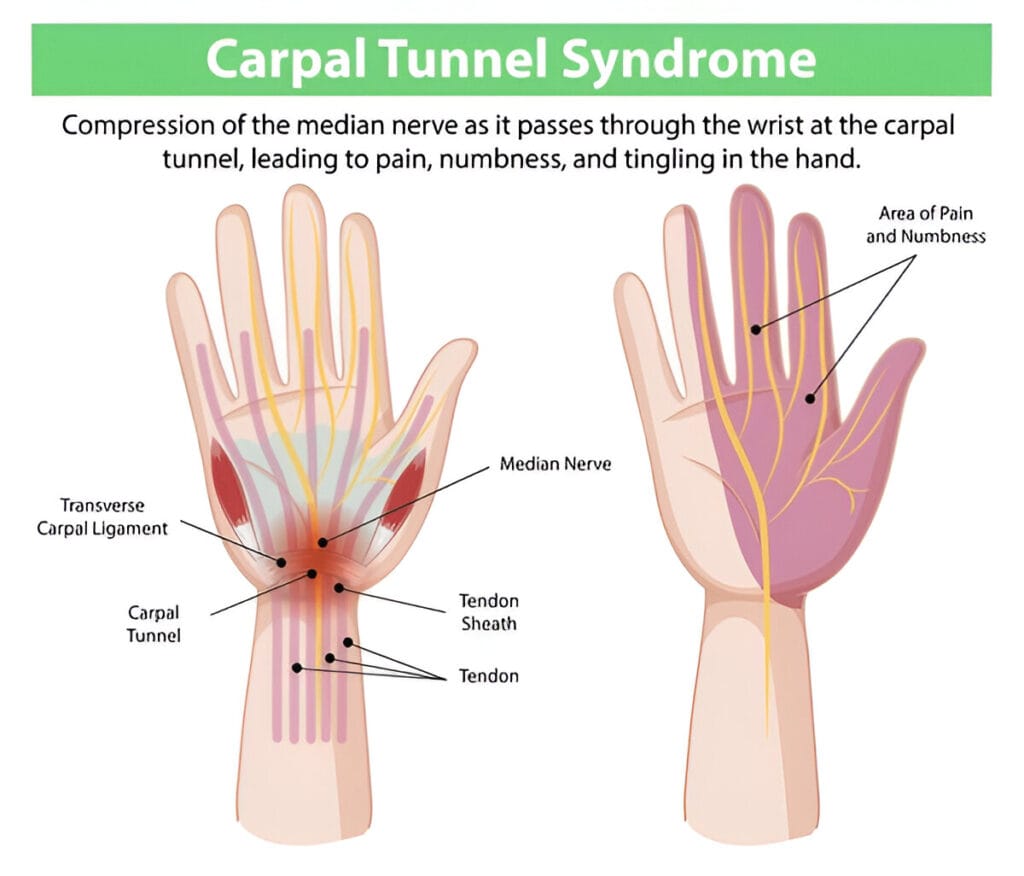
CTS is caused by compression of the median nerve, which runs from your forearm into your palm through the carpal tunnel—a narrow passage in your wrist. Inflammation or swelling in this area pinches the nerve, leading to tingling, numbness, pain, and weakness in the hand.
It’s common among people who perform repetitive hand movements, such as typing, assembly work, or playing instruments. However, underlying conditions like diabetes, arthritis, or thyroid disorders, as well as pregnancy or genetic predisposition, can also play a role.
Early symptoms often start with nighttime numbness or a weak grip. If left untreated, CTS can lead to permanent nerve damage and muscle loss.
Why Early Awareness Matters
Many people don’t consider wrist health until symptoms appear. But CTS affects more than just the wrist—it can disrupt sleep, reduce productivity, and interfere with everyday tasks. Early intervention can prevent serious complications and reduce the need for surgery.
Taking simple steps, like improving ergonomics or taking regular breaks, can help protect your wrists and maintain your quality of life.
Anatomy and Vulnerability of the Carpal Tunnel
The carpal tunnel is a tight space in the wrist surrounded by bones and ligaments. It houses the median nerve and tendons that control finger movement. Because there’s little room to accommodate swelling, any inflammation can compress the nerve.
Modern lifestyles involving frequent typing, texting, or gaming increase stress on this area. Poor posture, repetitive motion, or health issues can worsen the problem, triggering CTS symptoms.
Understanding this structure explains why CTS is so common and how minor changes in wrist use can lead to major discomfort.
Common Causes and Risk Factors
Repetitive Hand Movements
Frequent, repetitive use of the hand is a major cause of CTS. Jobs involving constant typing, gripping, or tool use, like mechanics, chefs, or hairstylists, are at high risk. These actions create small injuries in wrist tissues that swell over time, narrowing the carpal tunnel.
Even hobbies like knitting or gaming, and daily smartphone use, can strain the wrist. Without breaks and proper ergonomics, symptoms can easily develop.
The solution? Break up repetitive tasks with rest, stretches, and posture adjustments to keep your wrists healthy.
Medical Conditions That Contribute to Carpal Tunnel Syndrome
Carpal Tunnel Syndrome (CTS) isn’t always caused by repetitive tasks. Several medical conditions can also raise your risk by causing inflammation, fluid retention, or nerve damage—compressing the median nerve in the wrist.
For example,
- diabetes increases the chance of nerve damage (peripheral neuropathy), making the median nerve more sensitive.
- Rheumatoid arthritis causes joint inflammation that can swell tendons in the carpal tunnel.
- Hypothyroidism and kidney disease can lead to fluid buildup, narrowing the tunnel space.
- CTS is also common during pregnancy due to hormonal swelling, though symptoms often improve after childbirth.
When these conditions combine with repetitive hand use or poor ergonomics, the risk multiplies. If you have any of these conditions, watch for early signs of CTS and seek medical advice promptly.
Genetic and Anatomical Risk Factors
CTS can also be inherited. Some people are born with a narrower carpal tunnel, which leaves little room for swelling before nerve compression begins. Factors like wrist shape, tendon size, and ligament thickness often run in families.
Injuries such as a broken wrist or dislocation can also reshape the tunnel, creating long-term nerve pressure. Even minor misalignments may worsen over time.
Age and Lifestyle
Aging reduces tissue elasticity, making older adults more vulnerable. Poor posture, inactivity, and smoking also contribute.
Recognizing these risk factors is key to both prevention and early intervention.
Symptoms of Carpal Tunnel Syndrome
Early Signs
CTS often begins subtly. Numbness or tingling in the thumb, index, middle, and part of the ring finger—especially at night—is common. You might wake up with a “sleeping” hand or feel the urge to shake it out.
Other early symptoms include a pins-and-needles sensation, hand weakness, or clumsiness—like dropping things or struggling to open jars. These are early warning signs that shouldn’t be ignored.
Addressing symptoms early can make non-invasive treatments more effective.
Progressive Symptoms
Without treatment, CTS worsens. Numbness becomes constant and more painful. Discomfort may spread to the forearm or shoulder, especially during daily activities like typing or driving.
Grip strength may decline, and your hand may struggle with fine motor skills—making buttoning shirts or tying shoes harder. In severe cases, the base of the thumb can visibly shrink from muscle loss due to prolonged nerve damage—often requiring surgery.
When symptoms progress, ergonomic fixes aren’t enough. A medical evaluation is essential to avoid permanent damage.
When to See a Doctor
If symptoms persist for more than a few weeks or begin affecting your daily life, it’s time to see a doctor. Ongoing numbness, pain, or hand weakness—especially if sleep or work is disrupted—warrants professional help.
A proper diagnosis can confirm whether you have CTS or a different condition like arthritis or a neck-related nerve issue. Early medical attention improves your chances of avoiding surgery and long-term nerve damage.
Don’t rely on self-diagnosis. If your hands are acting up, listen to your body and get checked.
Diagnosing Carpal Tunnel Syndrome
Physical Exam and Symptom Check
Your doctor will ask about your symptoms, when they began, how often they occur, what makes them worse, and whether both hands are affected.
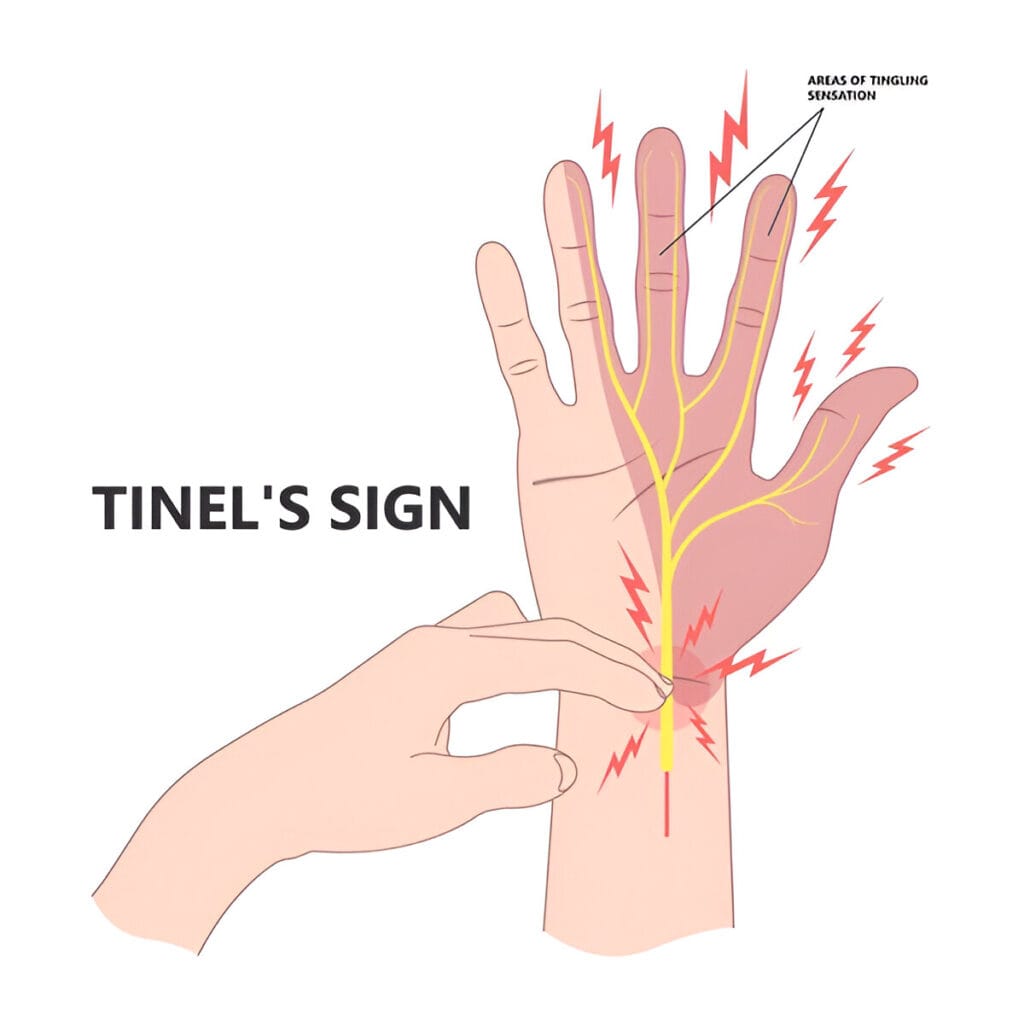
They’ll perform simple tests like
- The Tinel’s Sign (tapping the median nerve to check for tingling)
- The Phalen’s Maneuver (bending wrists together to trigger symptoms).
- Grip strength and signs of muscle loss, especially at the thumb base, are also evaluated.
Often, this hands-on assessment is enough for an accurate diagnosis. Clear communication about your symptoms helps guide effective treatment.
Nerve Conduction Studies & Electromyography (EMG)
Nerve conduction studies (NCS) check how fast signals travel along the median nerve. Slower signals indicate compression. Electromyography (EMG) measures how muscles respond to nerve signals using a fine needle electrode. This test can detect muscle damage from prolonged nerve compression.
These tests are safe, minimally invasive, and help distinguish CTS from other conditions like cervical nerve issues or peripheral neuropathy. They’re considered the gold standard for diagnosis and treatment planning.
Imaging and Other Diagnostic Tools
In some cases, imaging helps clarify the diagnosis.
- Ultrasound is a common, painless option that shows median nerve swelling or compression. It can also reveal cysts or tendon problems.
- MRI is used in complex cases to examine soft tissues in detail—helpful when surgery is considered or the diagnosis is uncertain.
- X-rays may be ordered to rule out bone spurs, fractures, or arthritis that could narrow the carpal tunnel.
Occasionally, blood tests are used to check for underlying issues like diabetes, rheumatoid arthritis, or thyroid disorders that may contribute to symptoms.
While not always necessary, these tools ensure accurate diagnosis and targeted treatment.
Non-Surgical Treatments
Lifestyle and Ergonomic Changes
Many CTS cases improve without surgery. Early to moderate symptoms often respond well to lifestyle changes and ergonomic adjustments.
- At work, your wrists should stay straight, with keyboards at elbow height. Wrist rests and ergonomic devices can reduce strain. In hands-on jobs, avoid bending or overextending your wrists.
- Take regular microbreaks every 20–30 minutes to stretch, shake out tension, and reset posture. Simple changes, like not sleeping with bent wrists or adjusting your grip on tools, can prevent symptoms from worsening.
- At home, use cold packs to reduce swelling or heat to relax stiff muscles. Wearing splinting gloves at night keeps wrists in a neutral position, easing nighttime symptoms.
These small shifts can significantly reduce CTS flare-ups and promote recovery.

Wrist Splints and Bracing
Wrist splints are a low-cost, non-invasive option that help keep your wrist in a neutral position, relieving pressure on the median nerve—especially at night when unintentional bending is common.
Nighttime splinting is often the first treatment step and can quickly reduce tingling and numbness. Daytime braces that limit extreme movement while allowing functionality may also help during repetitive tasks.
There are different types—rigid or flexible—depending on your needs. Braces are drug-free and safe for all, including pregnant women.
Wearing splints during activities like typing, gardening, or driving can prevent strain and reduce the risk of worsening symptoms. Consistent use improves outcomes and can help avoid more invasive treatments later.
Medications and Corticosteroid Injections
When wrist splints and lifestyle changes aren’t enough, medications may help manage Carpal Tunnel Syndrome (CTS) symptoms. Over-the-counter NSAIDs like ibuprofen or naproxen can reduce wrist inflammation and relieve pain—especially during flare-ups—but they don’t treat the underlying nerve compression.
For more direct relief, doctors may recommend corticosteroid injections into the carpal tunnel. These powerful anti-inflammatory drugs reduce swelling around the median nerve and often bring fast, temporary relief—sometimes lasting months. They’re useful for postponing surgery or managing symptoms before an important event. However, repeated injections may weaken surrounding tissues, so usage is typically limited.
In some cases, oral steroids or diuretics are prescribed, particularly when CTS is linked to systemic issues like arthritis or fluid retention.
While not a cure, medications can be a key part of a broader, non-surgical treatment plan.
Surgical Treatment – Carpal Tunnel Release
Open vs. Endoscopic Surgery
When conservative treatments fail, Carpal Tunnel Release Surgery is often the next step. The procedure involves cutting the transverse carpal ligament to relieve pressure on the median nerve.
There are two main surgical methods:
- Open Surgery: A small incision is made in the palm, allowing the surgeon to directly cut the ligament. It’s widely used and especially effective for severe cases.
- Endoscopic Surgery: A less invasive option using a small camera and instruments inserted through one or two tiny incisions. It typically results in quicker recovery and less pain.
Both have high success rates (over 90%). The best option depends on the surgeon’s experience and your specific needs.
What to Expect: Before, During, and After Surgery
Before surgery, your doctor will confirm the diagnosis with tests like EMG or ultrasound and review anesthesia options—usually local or regional.
During the 15–30-minute procedure, the surgeon cuts the transverse ligament to relieve nerve pressure. You’ll remain awake but won’t feel pain.
After surgery, you can usually go home the same day. Keeping the wrist elevated and using over-the-counter pain relief helps manage swelling and discomfort. Many notice symptom improvement within days.
Recovery varies: most return to light tasks in 1–2 weeks and resume full activities in 4–6 weeks. Physical therapy may be suggested for severe cases to regain strength and mobility.
Success depends on following aftercare instructions and avoiding overuse during healing.
Success Rates and Recovery
Carpal tunnel release is one of the most successful orthopedic surgeries, with a success rate between 85% and 95%. Most people experience a major drop in pain and tingling shortly after the procedure and regain full hand function.
Recovery time depends on the method:
- Open surgery: 4–6 weeks for heavier activity.
- Endoscopic surgery: 2–3 weeks for many tasks.
Most people recover with minimal therapy, though home exercises—like stretching and grip strengthening—can speed up results.
Surgery isn’t a guaranteed fix if root causes like repetitive strain or medical conditions remain unaddressed. But for most, it brings lasting relief and restores quality of life.
Long-Term Management and Prevention
Ergonomics and Healthy Habits:
- Keep wrists neutral at work
- Use ergonomic tools and maintain good posture
- Take microbreaks and stretch regularly
Daily Routines:
- Maintain a healthy weight and stay active
- Quit smoking to improve circulation
- Watch for early signs and adapt activities accordingly
Home Care:
- Alternate cold and warm compresses
- Use wrist braces during activities and sleep
- Apply topical pain relievers as needed
Mind-Body Support:
- Practice stress-relief techniques like meditation
- Connect with support groups or communities
Living with CTS
Managing CTS is about adapting daily habits and using the right tools. Whether it’s using ergonomic kitchenware, relying on voice-to-text apps, or incorporating daily stretches, small adjustments can make a big difference.
Support from friends, family, or online communities also helps you navigate the condition with more confidence and less isolation.
Final Thoughts
Carpal Tunnel Syndrome is manageable—and often preventable. Early action, smart habits, and the right care plan can help you avoid surgery or recover successfully from it.
With the right approach, you can protect your hands and maintain a pain-free, functional lifestyle.