What Is Capsulorrhaphy?
Capsulorrhaphy is a surgical procedure used for tightening the joint capsule of the shoulder to restore stability and prevent dislocations. This procedure is commonly done when someone experiences repeated shoulder dislocations, especially in younger, more active individuals. The shoulder joint, being the most mobile joint in the body, sacrifices some stability for a greater range of motion. When this mobility leads to recurring injuries, surgical solutions like capsulorrhaphy come into play.
In most cases, this procedure is paired with other corrective techniques, such as Bankart repair, to ensure a comprehensive solution to instability. The goal is simple: reinforce the shoulder so it doesn’t “pop out” again during activity. If you’ve ever had your shoulder dislocate during a simple movement like reaching backward, you’ll understand how crucial this stability is.
Capsulorrhaphy Definition and Meaning
The word “capsulorrhaphy” is derived from two parts: “capsulo,” referring to the joint capsule, and “rrhaphy,” meaning surgical suturing or repair. Essentially, capsulorrhaphy refers to the tightening or repair of a joint capsule, often through sutures, to limit excessive movement.
Common Conditions Treated with Capsulorrhaphy
Here are the most frequent situations where a capsulorrhaphy procedure is deemed essential:
- Anterior Shoulder Instability: The most common condition, usually caused by dislocations that push the arm forward and out of the socket.
- Bankart Lesion: A tear of the labrum that occurs due to repeated dislocations. Often corrected simultaneously with capsulorrhaphy.
- Multidirectional Instability (MDI): Seen in people whose joints are naturally loose. They may experience dislocations in multiple directions.
- Athletic Shoulder Injuries: Contact sports like football or activities involving overhead motion like baseball pitching often lead to repeated trauma on the shoulder capsule.
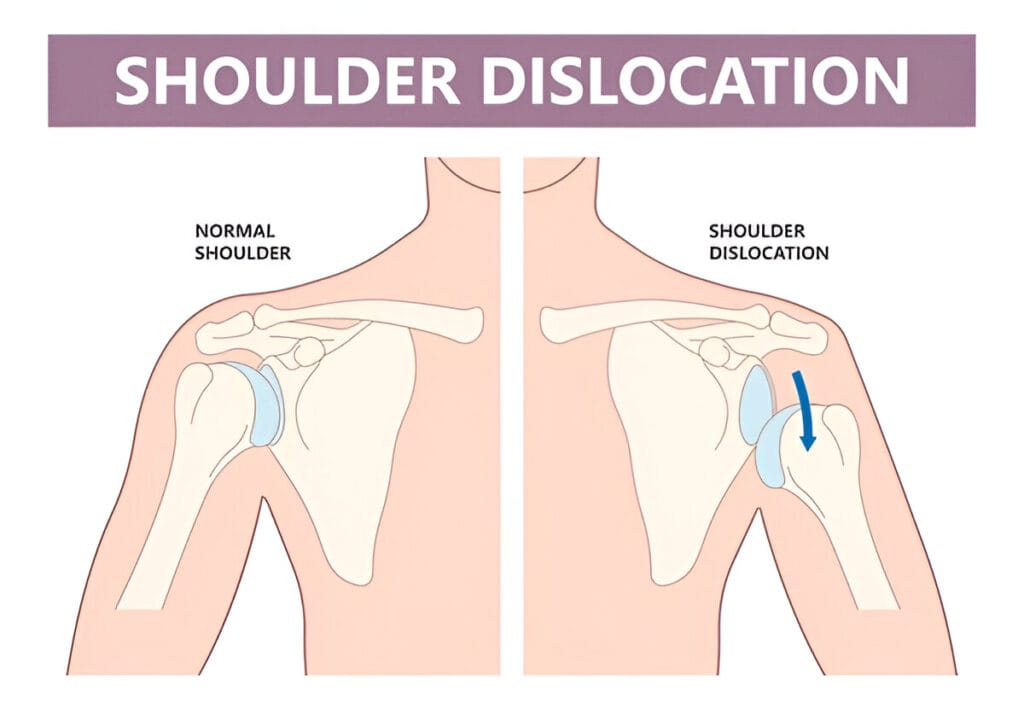
These conditions can dramatically affect daily life, not just athletic performance. Imagine not being able to reach for something on a high shelf or swing your arm without the fear of it popping out. Capsulorrhaphy is a step toward regaining control and confidence in your shoulder.
Related: What Is Glenohumeral Degenerative Joint Disease?
Open Capsulorrhaphy Shoulder Surgery
Open capsulorrhaphy is one of the traditional methods for correcting shoulder instability. Unlike arthroscopic techniques, this approach involves making a larger incision to gain full access to the shoulder joint. It may sound a bit intimidating, but for certain cases, it offers superior control and visualization for the surgeon, especially when dealing with complex or chronic instability.
So, why choose the open method? Typically, it’s recommended for individuals with:
- Recurrent, long-term shoulder instability
- Failed previous surgeries
- Extremely loose joint capsules
- High-demand shoulder use (e.g., manual laborers or overhead athletes)
The procedure starts with the surgeon making an incision in the front of the shoulder. Once inside, they examine the joint capsule and associated structures like the labrum and ligaments. If these structures are stretched or torn, the surgeon uses sutures to fold and tighten the capsule.
While arthroscopy offers a less invasive path, open capsulorrhaphy has a long track record of success. It allows for more direct manipulation of tissues, making it easier to customize the repair. Some studies even suggest that open procedures may offer lower recurrence rates in high-risk cases.
Arthroscopic Capsulorrhaphy
Arthroscopic capsulorrhaphy represents a more modern and minimally invasive method of repairing shoulder instability. It uses tiny incisions, a camera (arthroscope), and specialized surgical instruments to tighten the shoulder capsule. This method has become the gold standard for many cases, particularly among young athletes and individuals who prefer less downtime.
Here’s how it works: The surgeon inserts a camera into the shoulder joint to get a clear view on a monitor. Through additional small incisions, they use tools to place sutures that “pucker” the loose capsule and tighten it. The result? A more stable shoulder with minimal trauma to surrounding tissues.
Benefits of arthroscopic capsulorrhaphy include:
- Smaller incisions and less scarring
- Lower risk of infection
- Faster initial recovery
- Outpatient procedure (you go home the same day)
One important thing to note is that the surgeon may also perform additional procedures during the arthroscopy, such as repairing a labral tear (Bankart lesion) or removing loose tissue. That makes it a highly versatile technique.
Surgical Arthroscopy of the Shoulder with Capsulorrhaphy CPT Code
For patients or medical coders looking into insurance claims or billing, the correct CPT (Current Procedural Terminology) code is critical. The CPT code used for surgical arthroscopy of the shoulder with capsulorrhaphy is typically 29806.
This code covers arthroscopic shoulder surgery that includes:
- Repair of the joint capsule (capsulorrhaphy)
- Treatment of labral tears (e.g., Bankart repair)
- Addressing anterior instability
It’s important for patients to know that this procedure may be listed under different codes if additional repairs or procedures are performed. For instance, if a SLAP tear is also repaired or bone spurs are removed, other codes may be included on the surgical billing.
When reviewing surgical paperwork or insurance documents, you’ll often see “arthroscopic capsulorrhaphy (CPT 29806)” listed alongside descriptors like “anterior stabilization” or “labral repair.” If you’re unsure about what’s covered under your insurance, it’s a good idea to speak directly with your provider or the billing department.
The CPT code isn’t just paperwork—it reflects the complexity and scope of your surgery. Understanding it gives you better insight into both the medical and financial aspects of your treatment.
Capsulorrhaphy vs Capsulotomy
It’s easy to confuse the terms capsulorrhaphy and capsulotomy—they sound similar but serve opposite purposes. Understanding the difference can help you better navigate discussions with your doctor and know what treatment you’re undergoing.
Let’s break them down:
- Capsulorrhaphy involves tightening the joint capsule. It’s performed to correct instability by reducing excess movement.
- Capsulotomy, on the other hand, involves cutting or loosening the capsule. It’s typically done when motion is restricted, such as in cases of frozen shoulder or joint stiffness.
So, if you’re dealing with a shoulder that pops out too easily or feels loose, your surgeon will likely recommend capsulorrhaphy. But if your shoulder feels “locked” or has severe limitations in movement, capsulotomy may be the better route.
Bankart Repair with Capsulorrhaphy
When it comes to shoulder dislocations—especially anterior ones—a common underlying issue is a Bankart lesion. This injury involves a tear in the labrum, the soft cartilage rim that surrounds the shoulder socket. When this occurs, it compromises shoulder stability, making dislocations more likely to recur. That’s where Bankart repair with capsulorrhaphy comes in as a powerful combo procedure.
During surgery, the torn labrum is reattached to the bone using anchors and sutures—this is the “Bankart repair” portion.
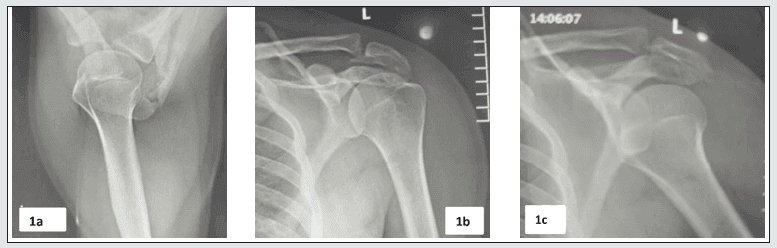
To ensure long-term stability, the surgeon also performs capsulorrhaphy—tightening the overstretched capsule to keep everything snug. The combo approach is particularly effective for:
- Young athletes under 30
- Those with multiple dislocations
- High-demand individuals (military, manual laborers)
- People with generalized ligament laxity
By addressing both the labral tear and the loose capsule, this technique drastically reduces the risk of another dislocation. Most modern orthopedic surgeons now favor the dual repair approach to tackle shoulder instability head-on.
Recovery from this procedure typically involves sling immobilization, followed by a multi-phase rehabilitation program (more on that shortly).
Rehabilitation Protocol for Bankart Repair
Getting surgery is just the beginning. The real game-changer is rehab—and the rehabilitation protocol for Bankart repair with capsulorrhaphy is key to a full and safe recovery. This carefully designed roadmap ensures your shoulder heals correctly, regains strength, and returns to full function without reinjury.
The protocol is generally broken down into four phases, each with its own set of goals and restrictions. Here’s a breakdown of what to expect:
Phase 1: Protection and Immobilization (Weeks 0-4)
- Goals:
- Protect surgical repair
- Control pain and inflammation
- Maintain hand, wrist, and elbow mobility
- What You’ll Do:
- Wear a sling 24/7 (except during prescribed exercises)
- Gentle pendulum exercises
- Isometric shoulder exercises (no active shoulder motion)
During this period, rest is crucial. Overdoing it now can compromise the surgical repair.
Phase 2: Early Mobility (Weeks 4-8)
- Goals:
- Restore passive range of motion (ROM)
- Gradually reintroduce active movements
- Avoid stressing the anterior capsule
- What You’ll Do:
- Passive and assisted ROM (with a therapist)
- Begin active ROM around 6 weeks (no resistance)
- Scapular stabilization exercises
This phase builds a gentle bridge between rest and motion. Consistency, not intensity, is the name of the game.
Phase 3: Strengthening (Weeks 8-16)
- Goals:
- Improve muscle strength and endurance
- Normalize movement patterns
- Increase functional range
- What You’ll Do:
- Resistance band and light dumbbell training
- Proprioception and balance exercises
- Sport-specific movements (if applicable)
This is where strength returns—and confidence starts to grow.
Phase 4: Return to Activity (Months 4-6+)
- Goals:
- Resume full activity/sports
- Prevent reinjury
- Finalize neuromuscular control
- What You’ll Do:
- Advanced strengthening
- Plyometric drills (throwing, catching, etc.)
- Simulated sport movements
Return to play usually happens around 5 to 6 months post-op, depending on progress and surgeon approval.
A proper rehab protocol is just as important as the surgery itself. Without it, even the best surgical repairs can fail. That’s why your commitment post-surgery will ultimately determine the long-term outcome.
Capsulorrhaphy Shoulder Rehab Protocol
The capsulorrhaphy shoulder rehab protocol mirrors the Bankart protocol in many ways but can be uniquely customized depending on the patient’s baseline condition and the type of surgical repair performed (open vs arthroscopic). Rehab plays a pivotal role in restoring joint integrity, muscle balance, and functional range of motion.
Immediate Postoperative Care (Weeks 0-4)
- Key Objectives:
- Immobilize the shoulder to protect the surgical site
- Minimize inflammation and discomfort
- Prevent stiffness in adjacent joints
- Patient Tasks:
- Wearing a sling constantly
- Cold compresses for swelling and pain
- Begin hand, wrist, and elbow movements
Therapists may begin passive shoulder exercises after the first week, under strict supervision.
Intermediate and Advanced Rehab Phases (Weeks 5-20)
- Weeks 5-8:
- Introduce gentle passive range of motion
- Focus on scapular stabilization
- Begin proprioception and balance drills
- Weeks 8-12:
- Transition to active-assisted and active ROM
- Start isometric strengthening exercises
- Begin functional training (lifting light weights, daily tasks)
- Weeks 12-20:
- Continue strengthening rotator cuff and deltoid muscles
- Sport-specific or job-specific drills
- Begin return-to-play assessments
Throughout rehab, it’s crucial to avoid excessive external rotation in the early stages, which could stress the repaired capsule. Slow and steady truly wins the race here.
A physical therapist guides every step, ensuring exercises are done correctly and safely. Patients are also educated about posture, ergonomics, and shoulder mechanics to prevent future injury.
Capsulorrhaphy Shoulder Recovery Timeline
Understanding the capsulorrhaphy shoulder recovery timeline is essential for setting realistic expectations. This isn’t a quick fix—it’s a long game that demands patience, discipline, and a strong commitment to physical therapy.
Let’s break down the recovery journey:
Weeks 0–4: Initial Healing Phase
During this period, the focus is on healing. The joint capsule and any associated labral repairs need to begin fusing properly.
- You’ll wear a sling 24/7 to prevent movement that could disrupt healing.
- Pain and swelling are managed with medications and cold therapy.
- Physical therapy begins with gentle passive exercises, mainly guided by a therapist.
- No active use of the shoulder yet—rest is critical.
Weeks 4–8: Mobility Returns
This is when patients start feeling less pain and more mobility.
- The sling is often phased out by week 6.
- Passive and assisted range of motion exercises increase.
- Active movement begins under the therapist’s supervision.
- Patients report feeling “stiff,” but that’s normal and temporary.
Weeks 8–16: Strength Building Begins
Now that the shoulder has regained some flexibility, the focus shifts to strengthening and coordination.
- Resistance exercises are introduced, using bands and light weights.
- Activities that mimic daily movements are practiced.
- Postural training becomes a key focus to avoid poor mechanics.
- Return to light job duties (like desk work) is usually allowed around this time.
Months 4–6+: Return to Activity
Here’s where things start to feel “normal” again.
- Full range of motion is usually achieved.
- Advanced strengthening continues, especially targeting the rotator cuff and scapular muscles.
- Athletes begin sports-specific training—throwing, hitting, lifting, etc.
- Many return to full sport or work activities around the 5–6 month mark, though some may need longer.
It’s important to note that healing isn’t always linear. Some people may hit recovery milestones faster, while others need more time—especially if complications arise or if the surgery was more extensive. Stick with the program, stay consistent, and communicate with your physical therapist. That’s the real secret to success.
Pain Management and Physical Therapy
While capsulorrhaphy provides the mechanical stability your shoulder needs, the journey isn’t painless. Managing discomfort and sticking to a structured physical therapy program are the two main pillars of a smooth recovery.
Managing Post-Surgical Pain
After surgery, you’ll likely experience:
- Dull aches or soreness around the incision
- Sharp pain when moving the shoulder
- Stiffness, especially in the morning
Here’s how to stay on top of it:
- Medication: Your doctor may prescribe NSAIDs, acetaminophen, or even short-term opioids.
- Ice Packs: These help reduce swelling and numb the area.
- Sleep Positioning: Most patients sleep upright or in a recliner with pillows supporting the arm.
- Relaxation Techniques: Meditation and breathing exercises can ease stress-related tension.
Don’t tough it out—managing pain effectively ensures you can participate fully in therapy and prevents compensatory movement patterns.
Role of Physical Therapy
Therapy isn’t optional—it’s a must. You’ll typically start seeing a physical therapist within a week of surgery, and the sessions will continue for 4 to 6 months. Here’s what they’ll help you with:
- Restoring Range of Motion: Without straining the repair.
- Regaining Strength: Especially in the rotator cuff, deltoid, and scapular muscles.
- Improving Joint Position Sense (Proprioception): To prevent future injuries.
- Functional Movements: So you can get back to everyday life and sport-specific activities.
Therapists will also watch out for signs of complications such as frozen shoulder or nerve irritation. The relationship between you and your physical therapist becomes one of the most important aspects of recovery. Trust the process, stay consistent, and don’t skip sessions.
Risks and Complications
Like any surgical procedure, capsulorrhaphy does come with risks, though serious complications are rare when performed by an experienced surgeon. It’s important to be aware of the potential pitfalls so you can spot early warning signs and take appropriate action.
Potential Surgical Risks
Some of the most common risks include:
- Infection: Though rare, it can occur around the incision or deep within the joint.
- Nerve Damage: Injury to nearby nerves during surgery could cause temporary or permanent numbness or weakness.
- Stiffness or Frozen Shoulder: Excessive scar tissue can lead to reduced range of motion.
- Recurrence of Instability: In some cases, the shoulder may still dislocate again if the capsule becomes loose over time or if the repair fails.
- Adverse Reaction to Anesthesia: This is rare but possible, especially in patients with underlying health conditions.
Knowing these risks helps you stay alert. Post-surgical checkups are essential for catching any issues early.
How to Minimize Recovery Issues
You can take steps to avoid complications and ensure a smoother recovery:
- Follow post-op instructions religiously—this includes wearing your sling, avoiding specific movements, and taking medications as prescribed.
- Attend all physical therapy sessions and never “self-progress” your exercises.
- Keep the surgical area clean and monitor it for signs of infection like redness, swelling, or drainage.
- Be patient. Overdoing it early is the fastest way to set your recovery back.
When in doubt, contact your surgeon or physical therapist. You’re not alone in this journey, and being proactive is the best way to avoid setbacks.
Conclusion
Capsulorrhaphy is a game-changing solution for those battling chronic shoulder instability. Whether performed alone or alongside procedures like Bankart repair, it offers long-term stability and restores confidence in shoulder movement. But surgery is only half the story—successful outcomes depend just as much on your rehab journey, your patience, and your commitment to recovery.
If you’re facing this surgery, arm yourself with knowledge, build a solid relationship with your therapist, and take the healing process one day at a time. Your shoulder is counting on you—and with the right care, it can come back stronger than ever.